Telemedicine takes off in Southern Nevada with rise of COVID-19
Las Vegas resident Chester Bailey had an appointment with his primary care doctor last week but never left his house.
That’s because Bailey — who turns 79 on May 1 — had a telemedicine appointment, his first visit with a doctor via videoconferencing.
When an employee at HealthCare Partners Nevada asked if he’d be OK with a telemedicine appointment, “I was actually shocked,” Bailey said. “I didn’t know they could do that stuff.”
Within the last month or so, more Las Vegas Valley medical offices have started offering telemedicine appointments in response to the COVID-19 outbreak — part of a nationwide trend that has seen an explosion in use of the technology. A big selling point is that many patients are uneasy about going to a doctor’s office because of the risk of getting infected or infecting others.
Some doctors and telemedicine experts say the COVID-19 outbreak is spurring more acceptance of telemedicine — a change that could have a long-lasting impact on the nation’s health care system.
COVID-19 is leading to people think differently about what a doctor-patient interaction should look like, said Dr. Marc Kahn, dean of the UNLV School of Medicine. “Prior to COVID, people didn’t think about telehealth. If people were sick, they went to the doctor.”
Many practices change after a crisis as people see opportunities to do things in a better way, he said. “I think telehealth is just one of those things because it just makes more sense.”
Las Vegas Heart Associates — affiliated with MountainView Hospital — started offering telemedicine appointments for established patients a few weeks ago. New patients are still asked to come into the clinic for their initial visits.
Sisolak’s stay-home order a boost
Telemedicine took off in Nevada after Gov. Steve Sisolak’s stay-at-home order and social distancing guidelines, cardiologist Dr. Jeffrey Levisman said. “It’s an attempt to continue to provide medical care, especially for patients who are sick and elderly who are at a higher risk of getting the virus and (experiencing) a bad outcome.”
If an in-person appointment is canceled or pushed back to a later date, a patient’s condition may be left uncontrolled and that could turn into a hospital stay, Levisman said. “We want to minimize how many patients are going into the hospital besides (those with) COVID-19.”
Dr. Shadi Daoud, a cardiologist with Las Vegas Heart Associates, said he’s a big fan of telemedicine appointments and thinks they’re advantageous for both patients and medical providers. And he said he’s more efficient because he’s seeing more patients in a shorter amount of time.
Daoud sees mostly heart failure patients — many of whom are in their mid-60s to mid-80s and have limited mobility. Some live as far away as Pahrump and Bullhead City, Arizona.
That’s not to say there aren’t downsides to telemedicine.
Health care providers say the inability to do a physical exam and difficulty prescribing some controlled substances are both drawbacks. And, of course, patients who don’t have a smartphone or computer aren’t able to access the service. And with hackers scouring the internet for websites with security holes, patient privacy also is a big concern.
Billing for services also has been problematic. Previously there were strict federal requirements about where telemedicine could be used — it was often restricted to rural areas — and reimbursement rates were low for providers.
But the Centers for Medicare & Medicaid Services — the federal agency that administers Medicare and Medicaid — announced March 30 it is issuing new rules and waiving or relaxing other requirements to ease use of the service.
Not all medical issues can be addressed via telemedicine, though. That includes urgent conditions that need treatment or evaluation, such as chest pain. And some specialties, such as pediatrics, don’t always lend themselves to the virtual format.
Dignity Health officials announced March 23 the launch of Virtual Care Anywhere — a free on-demand telemedicine urgent care service for those experiencing mild or moderate symptoms similar to those of COVID-19 through its three St. Rose Dominican Hospitals in the Las Vegas Valley.
MountainView Hospital announced April 7 it’s providing telemedicine options for all of its outpatient clinics. Its parent company, HCA Healthcare, allows the use of platforms such as Healow (part of an online patient portal), FaceTime, Google Duo and Cisco WebEx Meetings to connect with health care professionals.
At Las Vegas Heart Associates, Levisman didn’t have an estimate of how many patients he has seen via telemedicine over the last few weeks. But just on the morning of April 9, it was nine of 10.
Levisman said telemedicine may play a role in the future for certain types of visits in his clinic once the COVID-19 outbreak passes, but it would be difficult to replace an in-person visit.
A majority of patients now seen online
Telemedicine isn’t new for the Southwest Medical group, which launched its NowClinic offering in 2014.
Previously it was used for on-demand appointments when distance or transportation was an issue. And more recently, it was used with specialty clinics, such as for chronic disease management.
But since March, “the need for (telemedicine) has exponentially increased,” said Dr. John Rhodes, senior medical director for the group.
Southwest Medical used to log about 70 on-demand visits in a 24-hour period. Now, it’s up to more than 400, with the majority of its appointments being done via telemedicine. That includes primary care, urgent care, behavioral health, hospice and specialists.
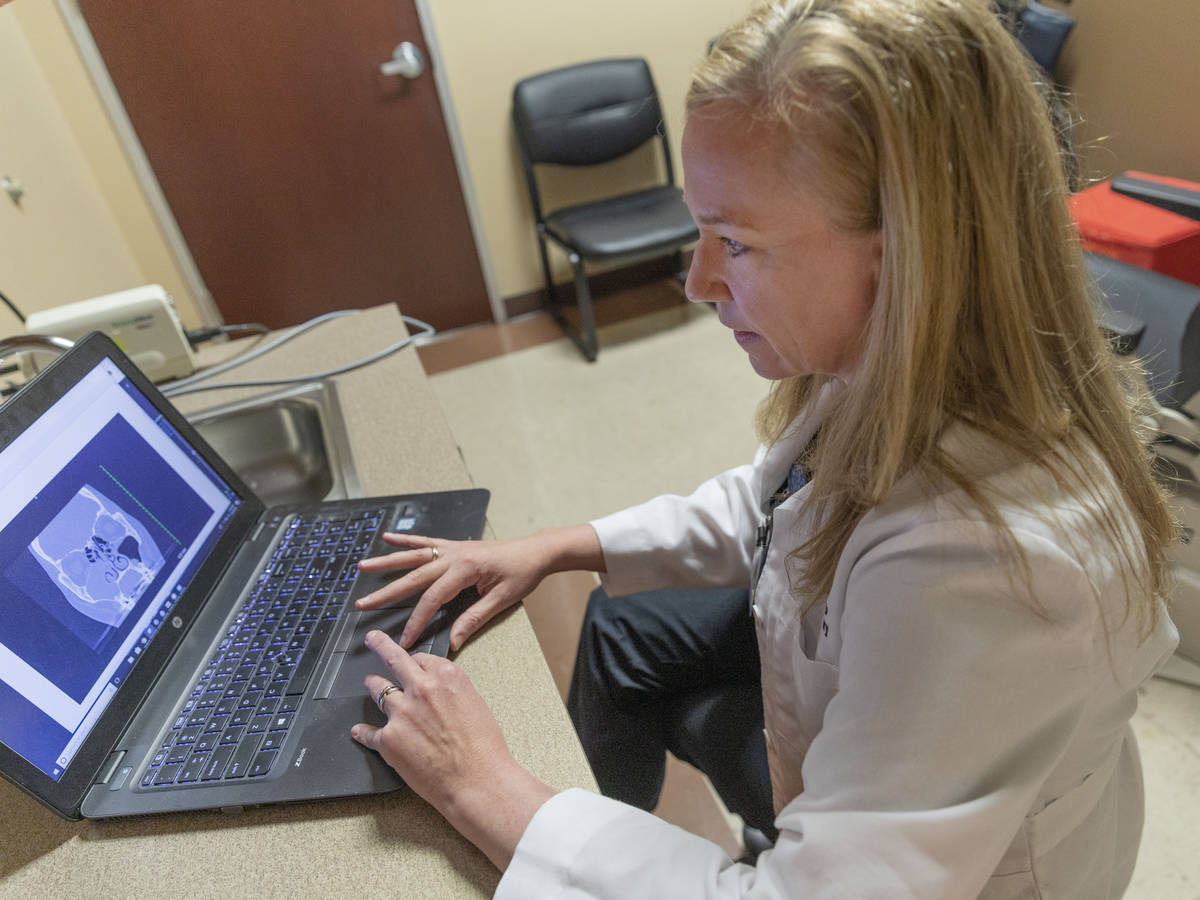
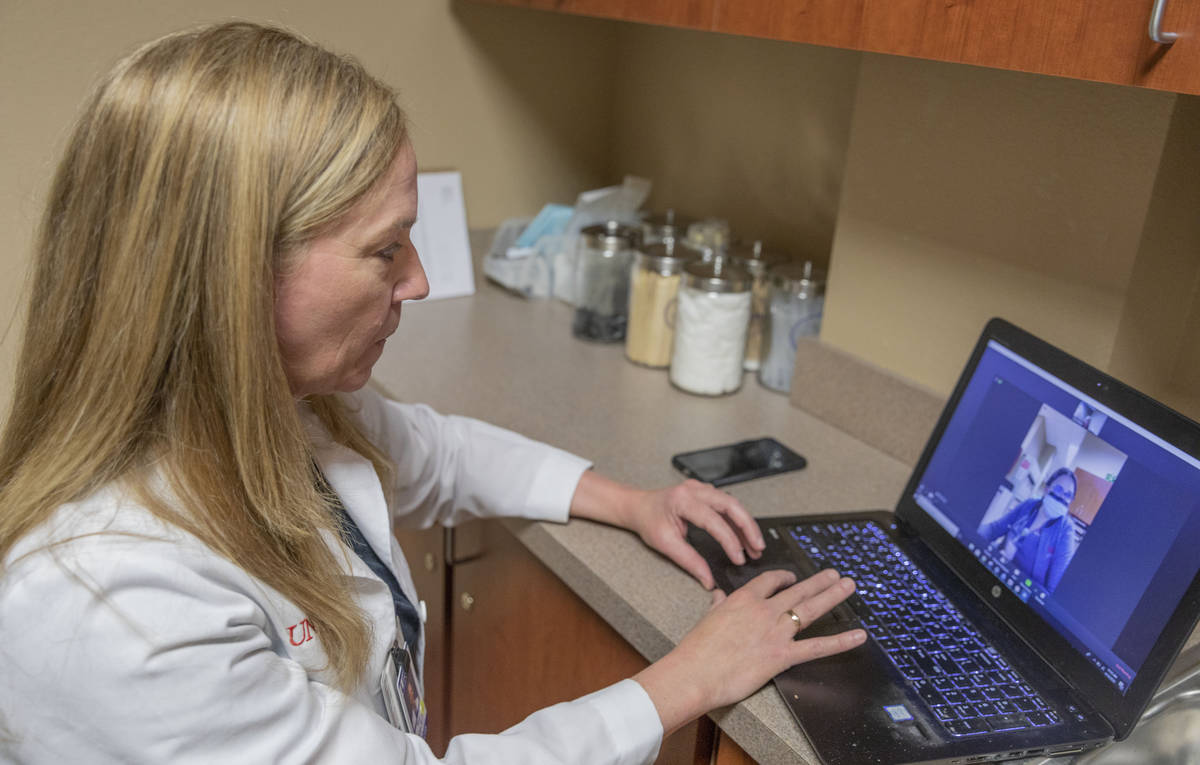
At UNLV Medicine, about 25 percent of appointments are being conducted via telemedicine — using a version of Zoom for medical providers that meets federal patient privacy requirements — since they were first offered about a month ago.
Dr. Michael Gardner, vice dean for clinical affairs at UNLV School of Medicine, said at least 10 percent of appointments will be provided via telemedicine once the COVID-19 outbreak passes — particularly, as a way to help patients who live in rural areas of the state.
Dr. Tina Elkins, assistant professor of general otolaryngology at the UNLV School of Medicine, said her ear, nose and throat patients are typically in the high-risk population for COVID-19, so most appointments have been transitioned to telemedicine using Zoom.
Patients may normally have an hour wait time in the clinic, but with telemedicine “we’re pretty much seeing them on their appointment time,” she said.
For certain acute or urgent issues — such as an outer ear infection — a patient needs to come in to be treated, she said.
Family Doctors of Green Valley — which has two clinics and seven medical providers — has offered telemedicine for about two weeks, and about 30 percent of appointments are in that format, medical director Dr. Ravi Ramanathan said.
HealthCare Partners Nevada — part of Utah-based Intermountain Healthcare — has offered telemedicine appointments for years, but adoption increased dramatically starting in mid-March.
Telemedicine went from being a “very small percentage of visits” to about two-thirds, President Mark Price said. “The pace of innovation and change in health care in the last month has been faster than anything I’ve seen in my career.”
HealthCare Partners Nevada is offering appointments by video or phone for both established and new patients. “We’re meeting the patient where they are and doing whatever what they’re comfortable doing,” Price said.
Bailey, who lives in senior housing in Spring Valley, said he was glad he didn’t have to go to his doctor’s office in person. “You don’t have to be there with someone who’s sick.”
Figuring out how to do an appointment via video was “simple stuff,” he said. “It was like seeing my doctor on television, you know?”
What the experts say
Center for Connected Health Policy is a Sacramento, California-based nonprofit that focuses on getting telemedicine technology into health care systems. Its three employees are scrambling to keep up with an influx of coronavirus-related requests for technical assistance.
The number of requests increased at least 20-fold in just two weeks, executive director Mei Kwong said. A lot of callers are “new people who never knew about telehealth before.”
“Telehealth has been around for a while and made some progress the last couple of years,” she said. “It has been going at a slow pace.”
But when COVID-19 hit, it led to stay-at-home orders across the nation and the need for ill patients to self-quarantine, so telemedicine has allowed for patients to receive care while staying in place, Kwong said.
Telemedicine also allows solo medical providers or small practices to survive economically by continuing to see patients, she said. “They need to basically stay afloat.”
Southwest Telehealth Resource Center, which provides a similar service, saw a 600 percent increase in requests for assistance in March, compared with the same month last year, co-director Elizabeth Krupinski said, adding most requests fall under the category of legal or financial.
There’s a question of what will happen with federal telemedicine regulations once the COVID-19 outbreak passes, Krupinski said, but she’s optimistic. “I hope the barriers stay fallen, but you never know.”
Contact Julie Wootton-Greener at jgreener@reviewjournal.com or 702-387-2921. Follow @julieswootton on Twitter.