Nevada ranks 8th for COVID-19 deaths, study says
A comprehensive new study of COVID-19 impacts lists Nevada as having the eighth-highest rate of death from the disease in the U.S.
The study, published Thursday in the Lancet medical journal, analyzed why rates of death were three or four times higher in some states than in others. It looked at many factors in each state, including implementation of pandemic restrictions, access to quality health care, education levels, vaccination rates and even political preferences.
To level the statistical playing field among the states, the rankings were adjusted for the age of the state’s population and prevalence of major underlying medical conditions. Without adjusting the data, Nevada had the 18th-highest death rate among the states and the District of Columbia, two of the study’s authors said in an interview.
Given that the population of Nevada is relatively young, the state “should have done better, because we know that COVID is so much more lethal for older populations,” said Joseph Dieleman, a study author and an associate professor of health metric sciences with the Institute of Health Metrics and Evaluation at the University of Washington.
The use by state governments of mask mandates and other pandemic restrictions was associated with lower levels of infections but not with lower death rates, the study found.
Higher vaccination rates were linked to both lower infection rates and lower death rates.
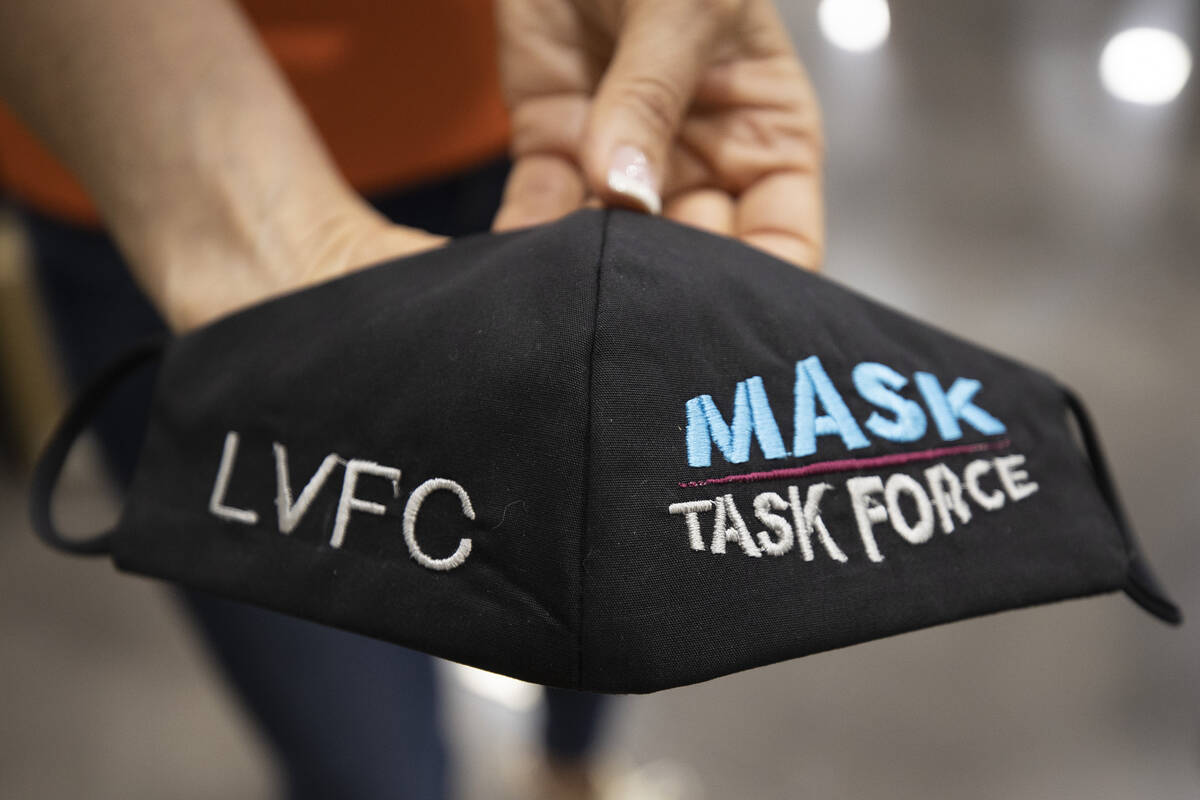
Emma Castro, co-lead author of the study, described Nevada as the biggest user of mask mandates of any state.
“They have been in place for the most amount of time during our study period, compared with the other states, and subsequently had very high mask usage, as well,” said Castro, a researcher with the Institute for Health Metrics and Evaluation. “But on the flip side, the vaccine uptake was quite low.”
Nevada ranked 41st for vaccine coverage, she said.
More than 2 years of data
Castro said Nevada was right in the middle among states when it came to poverty levels, levels of education and access to quality health care, factors that might improve a state’s COVID-19 outcomes.
“I think vaccines are probably playing one of the biggest factors in determining Nevada’s higher rates of death,” she said.
The study analyzed data from Jan. 1, 2020, to July 31, 2022, found in public databases. Among other findings were the following:
— The death rates were lowest in Hawaii, New Hampshire and Maine, and highest in Arizona, Washington, D.C., and New Mexico.
— States that imposed more vaccine and mask mandates experienced lower infection rates but tended to have worse employment rates and student test results, yet did not fare worse economically as measured by local gross domestic product.
— States with poorer, less-educated populations with less access to quality health care and less trust in others, as measured by surveys, experienced higher rates of infection and death.
— Higher public health spending and more public health personnel per capita were not associated, across the board, with fewer COVID-19 infections and deaths.
— Mandated restaurant closures and increased mask use were associated with larger decreases in employment rates. Less mask use, more infections and greater COVID-19 deaths were closely tied with higher employment.
— State-level school closures did not appear to play a role in lower student test results across most states. Instead, the study suggests that declines in fourth grade math were linked with several policy mandates, including increased mask use and vaccine mandates for state and school employees.
“It’s possible that in states that were more cautious about COVID-19 transmission, more parents elected for remote schooling. Another possibility is that mask and vaccine mandates impacted school attendance and closures in ways our study was not designed to measure,” co-lead author Thomas Bollyky, director of the Council on Foreign Relations’ Global Health Program, said in a news release.
— States with higher proportions of Black and Hispanic people were associated with higher death rates, reflecting local racial inequities, and health disparities.
— The political affiliation of a state’s governor was not associated with lower infection or death rates.
— Worse COVID-19 outcomes were associated with the proportion of a state’s voters who voted for the 2020 Republican presidential candidate, Donald Trump. This finding could reflect fewer pandemic protective restrictions and more vaccine hesitancy, Dieleman said.
Planning for next pandemic
Worse COVID-19 outcomes in the southeast are associated with “Republican states that have high poverty, low access to health systems, low trust,” he said. In connection with worse outcomes in the southwest, “we’re seeing a story that revolves around Hispanic people, lower vaccination rates … and lower insurance rates, as well.”
The findings are intended to assist public health officials in better planning for, and responding to, the next pandemic.
“Knowing where the outcomes are expected to be the worst is really powerful when planning for the next pandemic and allows us to be more prepared to provide more services and different sorts of communication in those communities specifically,” Dieleman said.
The study was funded by the Bill & Melinda Gates Foundation, J Stanton, T Gillespie, J and E Nordstrom and Bloomberg Philanthropies.
Contact Mary Hynes at mhynes@reviewjournal.com or 702-383-0336. Follow @MaryHynes1 on Twitter.