When the flu pandemic of 1918 hit, Las Vegas wasn’t spared




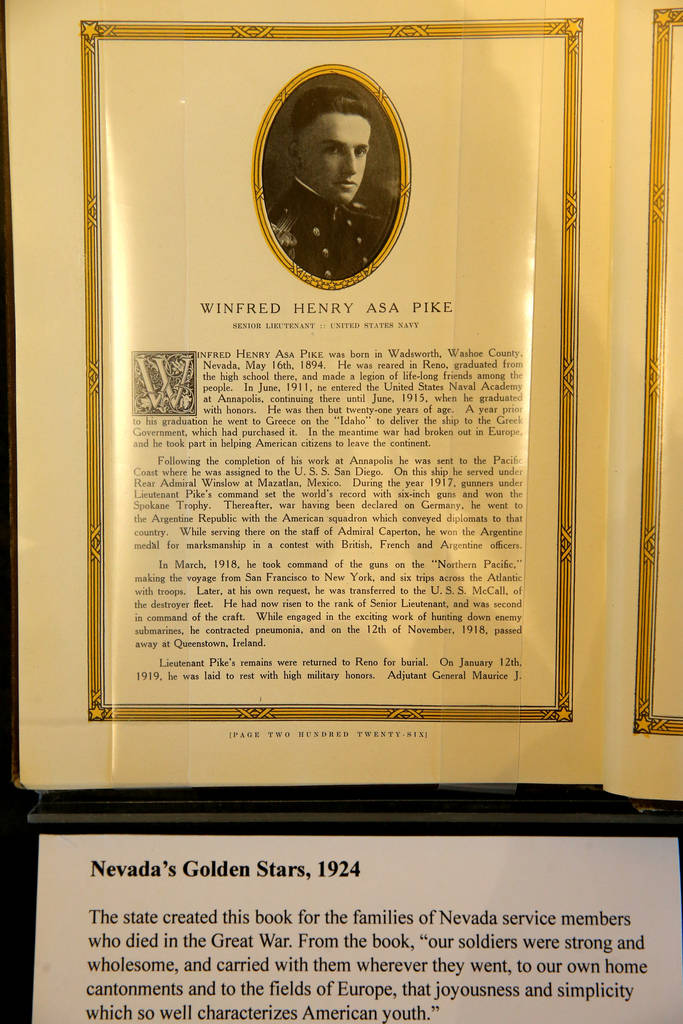

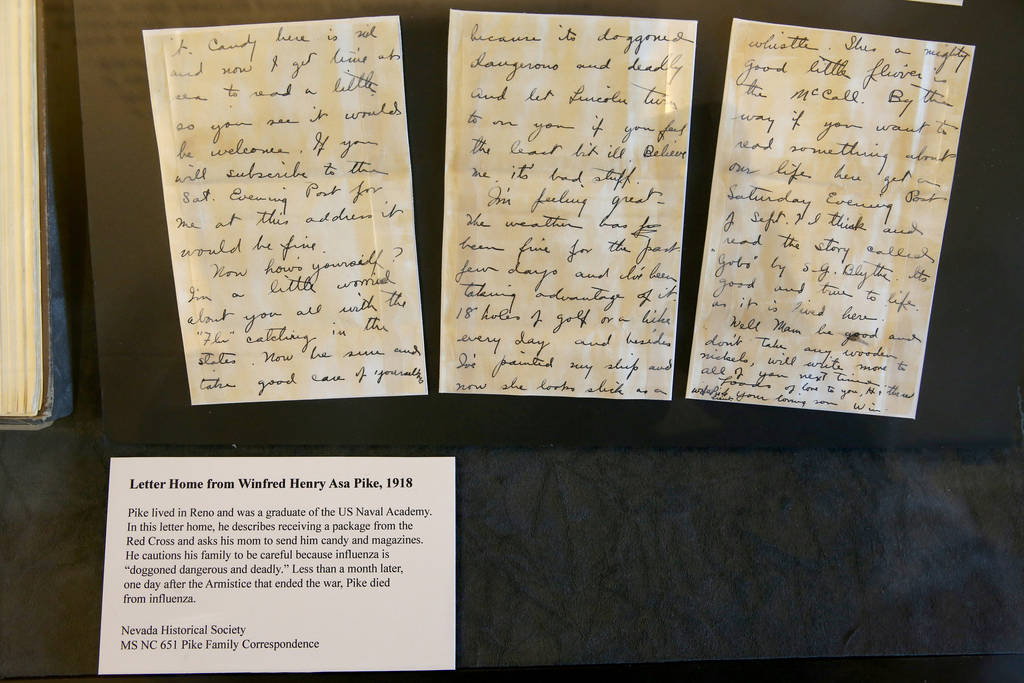
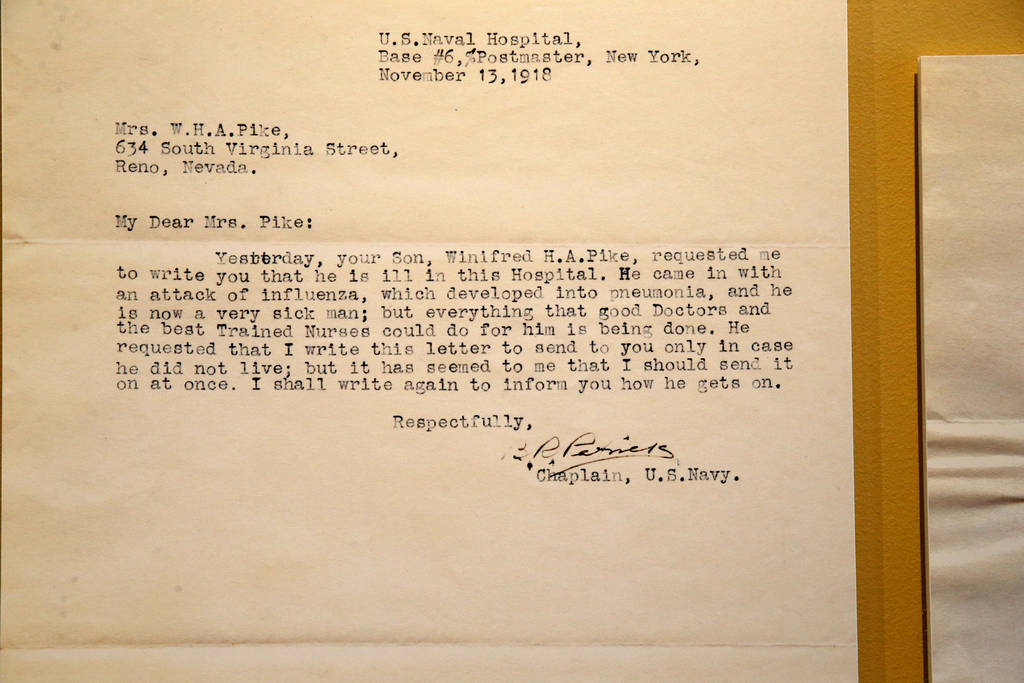
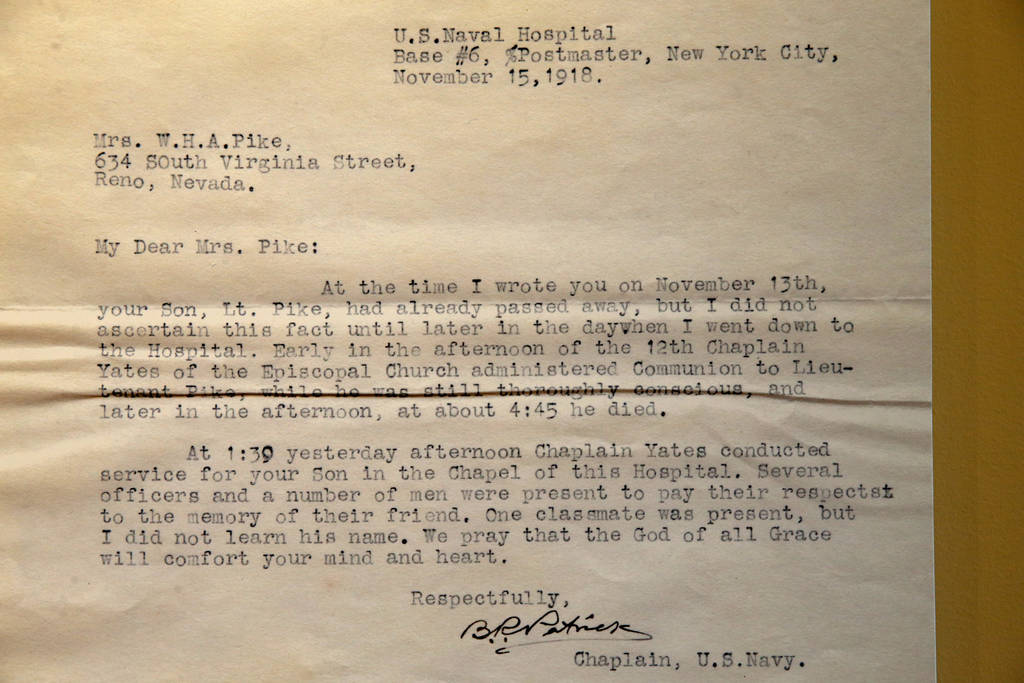




When Winfred Henry Asa Pike went off to fight in World War I, he surely knew that he might not return home to his family.
But what the Navy lieutenant and U.S. Naval Academy graduate from Reno couldn’t have imagined is that he would lose his life — not in battle, but to a fatal bout of influenza just one day after the armistice that ended fighting was signed.
That makes Pike a casualty of two concurrent world-changing events: World War I and the historic global influenza pandemic of 1918. This year marks the 100th anniversary of the flu epidemic, which the Centers for Disease Control and Prevention says remains, even today, one of history’s most deadly disease outbreaks.
500 million people
According to the CDC, about 500 million people — about one-third of the planet’s population — were infected with the influenza virus during the pandemic, which killed at least 50 million worldwide and about 675,000 in the United States.
The pandemic was so deadly, the CDC adds, that life expectancy in the United States was reduced by about 12 years — to just 36.6 years for men and 42.2 years for women — from 1917 to 1918.
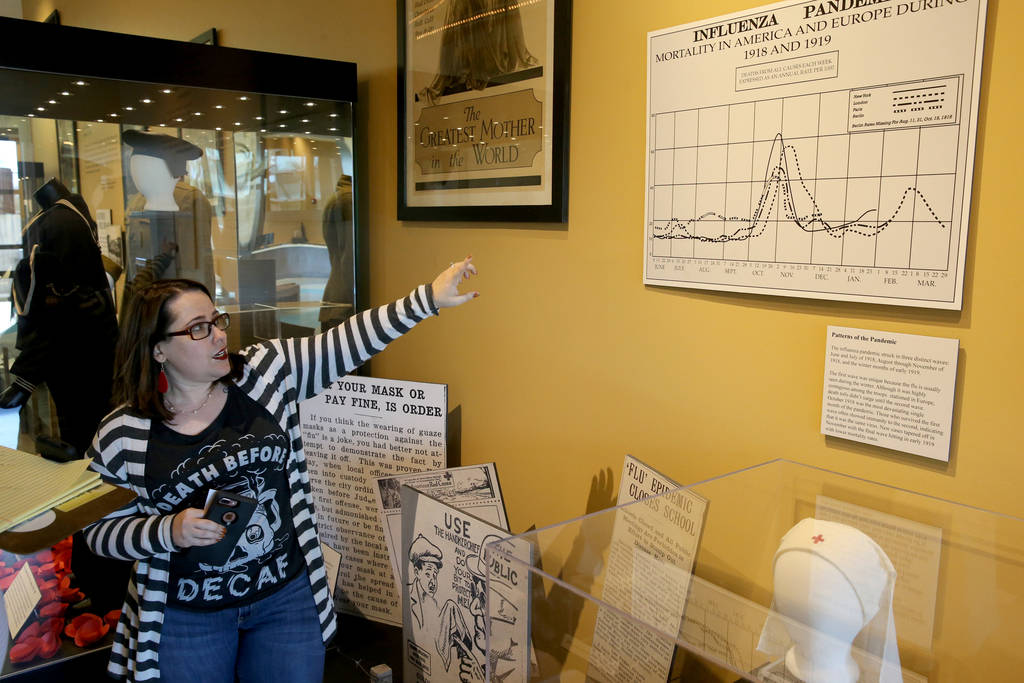
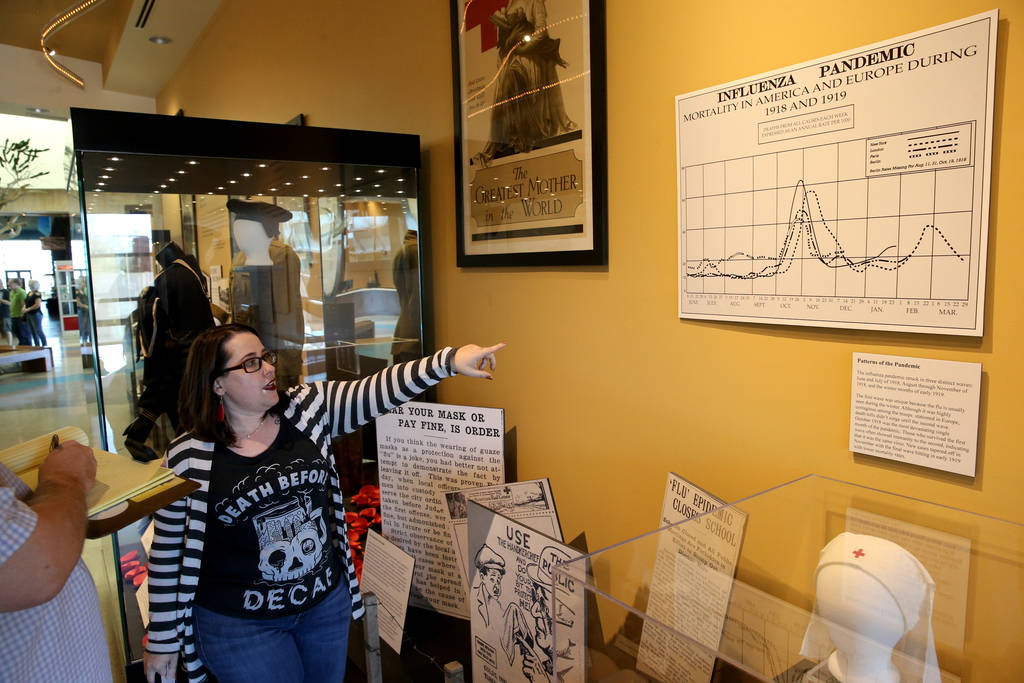
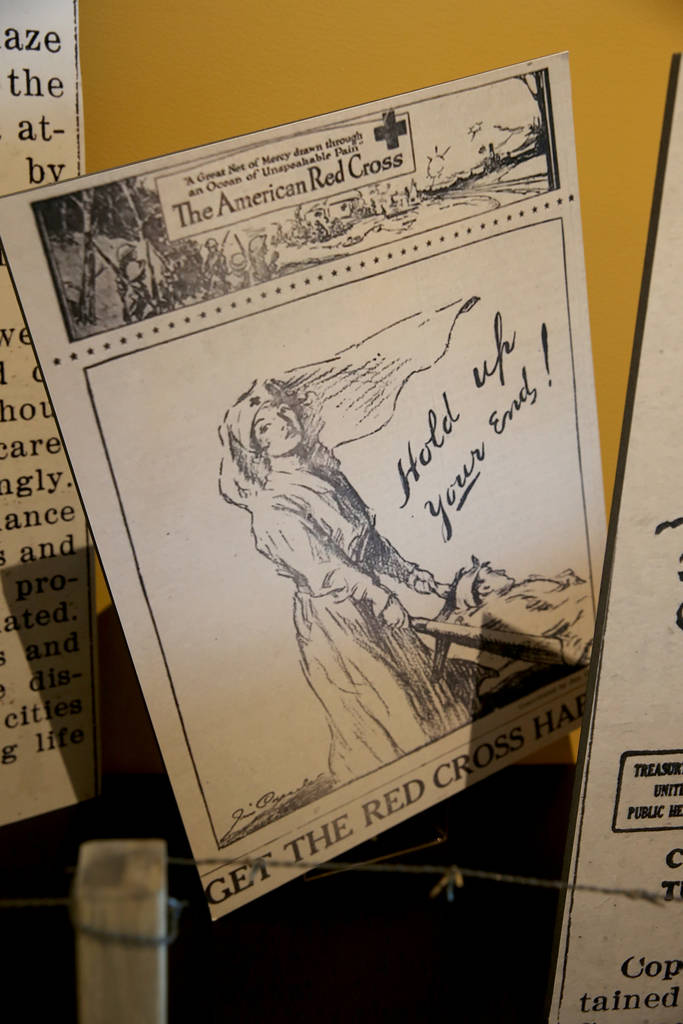
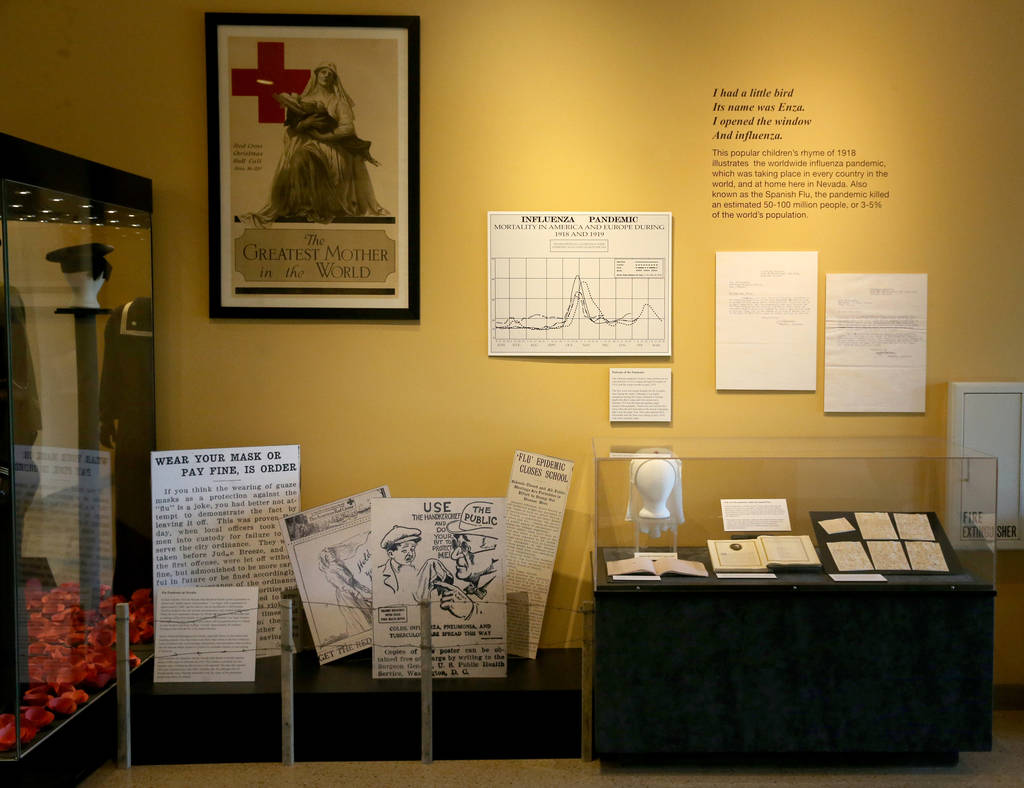
Of course, the pandemic didn’t leave Nevada untouched. Ilana Short of the Nevada State Museum Las Vegas researched the flu years here for an exhibition, “The Great War: The Western Front and the Nevada Homefront,” that runs through April at the museum and the Origen Museum at the Springs Preserve.
The pandemic officially caused about 40 deaths in Southern Nevada at a time when Las Vegas’ population was about 2,000, and the Nevada State Board of Health reported that the state saw almost 4,000 influenza cases in 1918.
But those numbers also may be artificially low. Flu cases were not required to be reported at the time, Short notes, and the death toll doesn’t take into account deaths from pneumonia — the state recorded 565 cases of pneumonia in 1918 — that may have been associated with the flu.
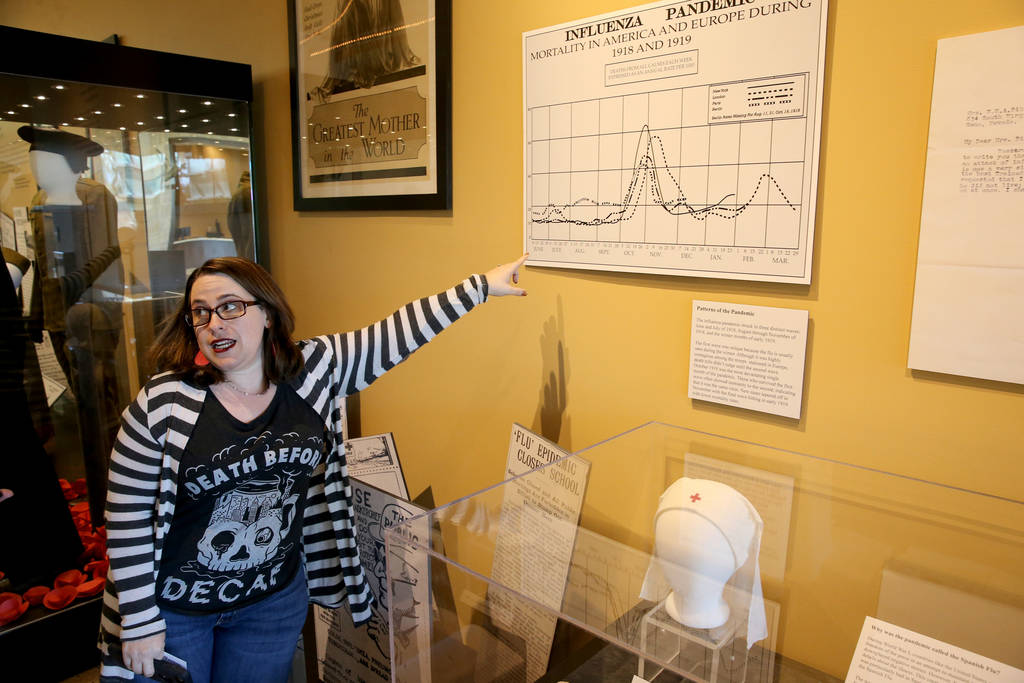
The pandemic began in the United States during the spring of 1918 and came in three waves that continued through winter 1918-19.The second wave was the most deadly.
“At some point the virus mutated, and when it mutated is when you start getting that huge wave,” Short says. “October and November of 1918 alone were the two deadliest months of the pandemic. Then you had a third and final wave in the winter (of 1919) that saw the same kind of symptoms, but we know it was the same virus because people who survived the first wave had immunity to the second two waves.”
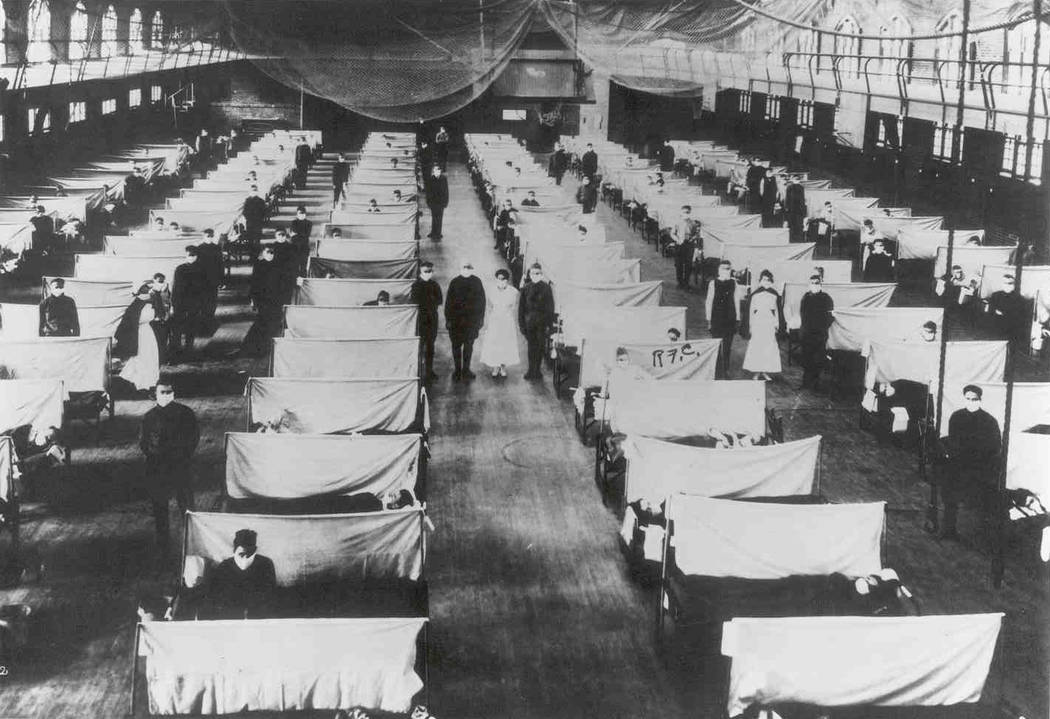
Various theories have traced the pandemic’s origin to locations that include a Kansas military camp and China. Whichever istrue, “the fact that the war was going on at the same time allowed it to spread quickly,” Short says, through war-related malnutrition in Europe, crowded battle trenches and military camps, and troop movements all over the globe.
The virus involved also targeted an unusual demographic group.
“We usually think of most (flu viruses) as affecting the very young and the very old and people in an immune-compromised situation, but this flu was the opposite,” Short says. “This was killing, proportionally, people between the ages of 15 and 45, more than any other age group.”
“There are stories of people walking down the street who just dropped dead,” she says, and of “kids going to bed at night and not waking up in the morning.”
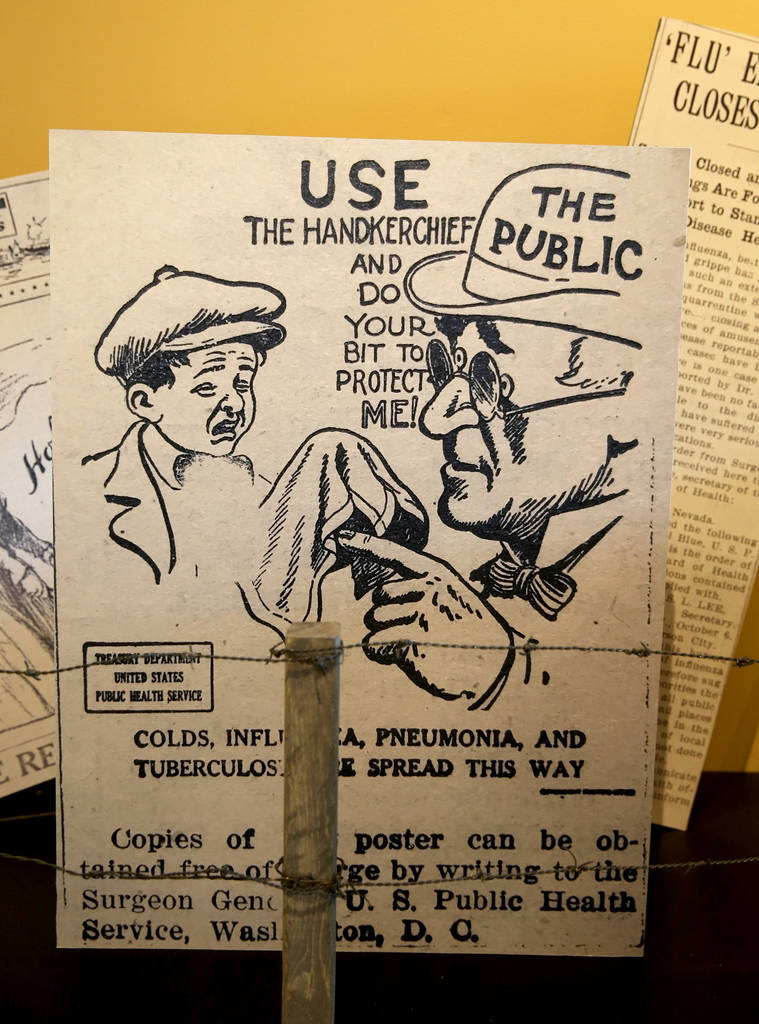
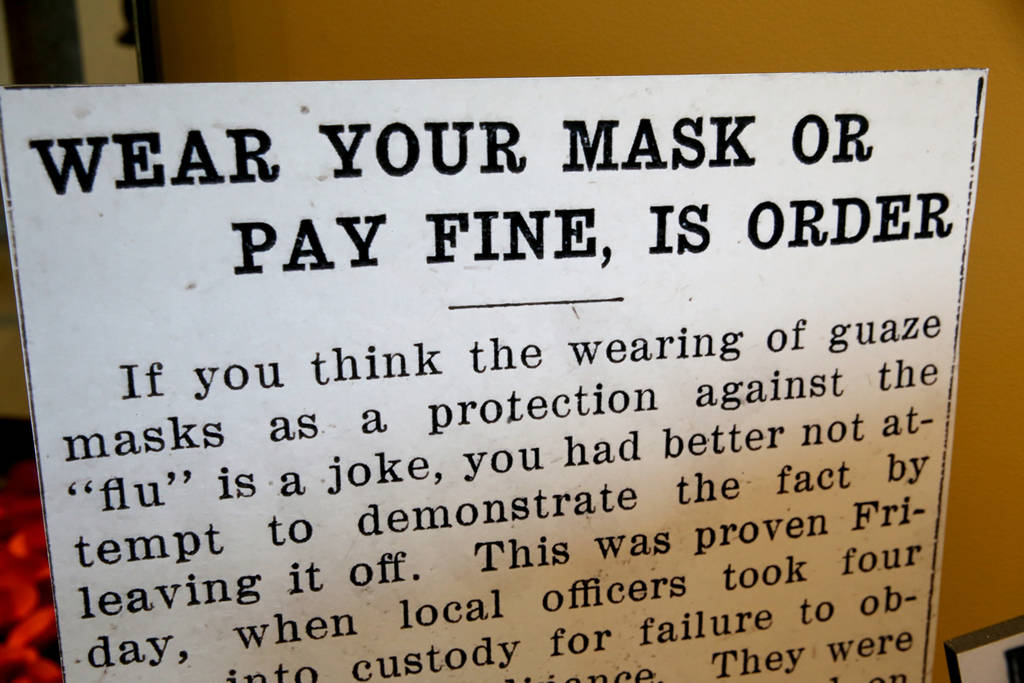
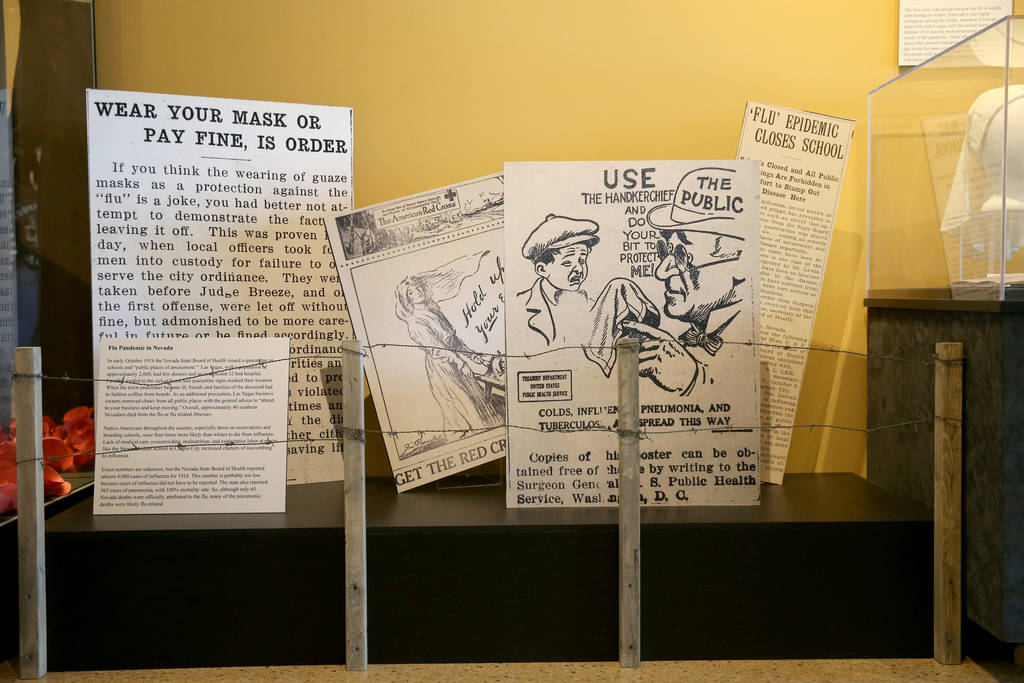
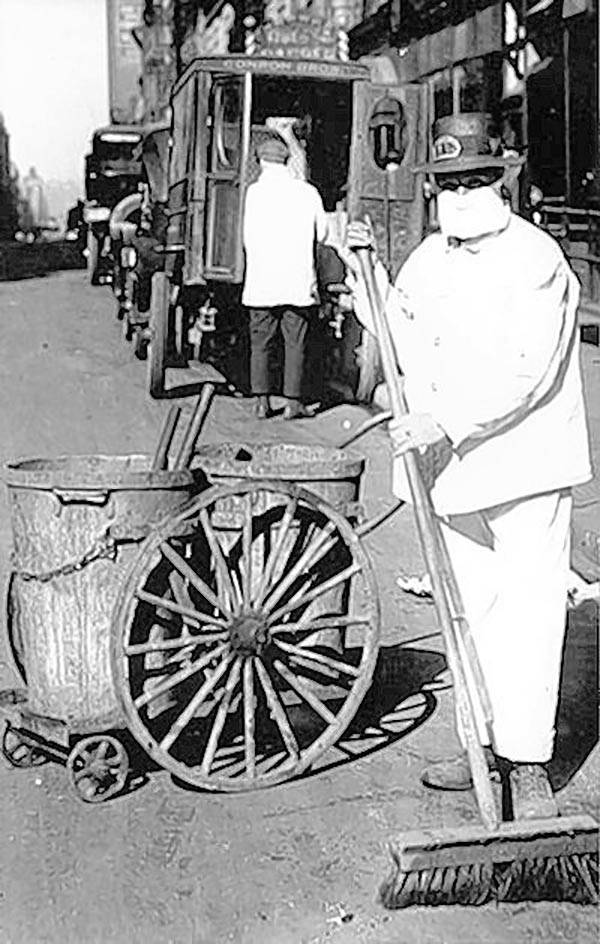
The flu hit hard during its second wave in September through November of 1918. The exhibition notes that Las Vegas’ city council adopted an ordinance requiring people to wear masks in public, and the Nevada State Board of Health in October imposed a quarantine on schools and “public places of amusement.”
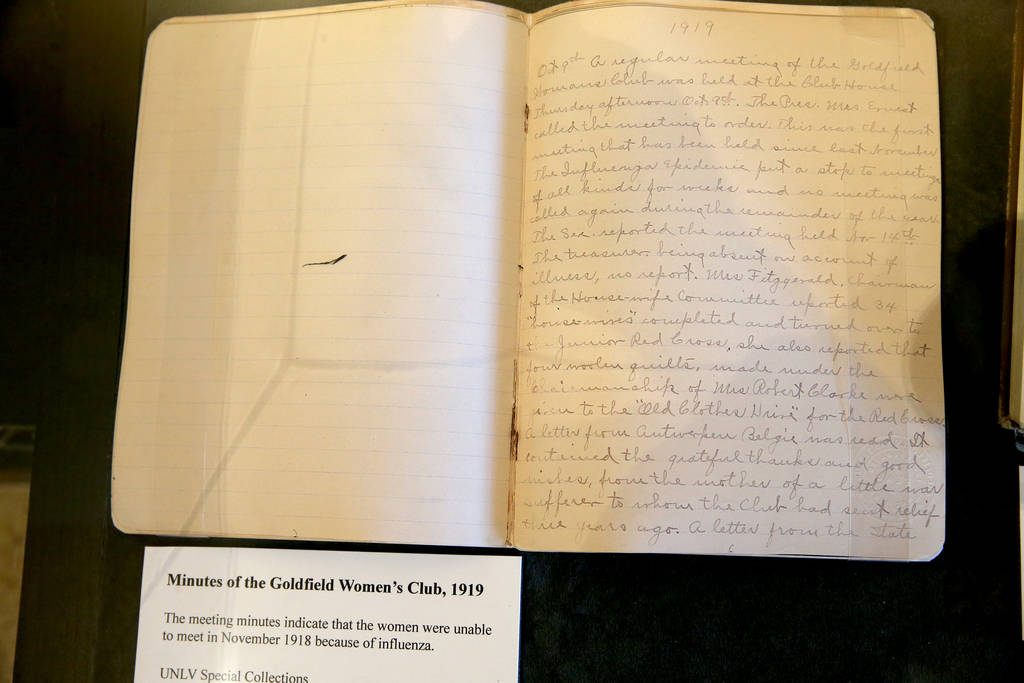
Meetings and public gatherings were canceled — the exhibit includes minutes of the Goldfield Women’s Club noting that its November 1918 meeting was canceled because of influenza — while merchants removed chairs from public places to reduce the incentive to linger unnecessarily.
Las Vegas at the time was home to just a 12-bed hospital and a handful of doctors, the exhibit notes. So families cared for flu victims in homes marked with quarantine signs, and when the city’s undertaker was stricken ill, friends and family members of flu victims resorted to building coffins out of boards.
Area newspapers, afraid of running afoul of laws that prohibited damaging morale, weren’t necessarily aggressive in covering the pandemic. During the war, according to the exhibit, the U.S. “suppressed the freedom of the press in an attempt to maintain morale” and newspapers “downplayed negative stories,” helping to give the flu an inaccurate common name.
“Because Spain was neutral, they could publish whatever they wanted,” Short says, and detailed reporting of the pandemic there “gave the rest of the world the perception that Spain was particularly hard-hit by the disease. That’s how it got the nickname ‘Spanish flu.’”
The pandemic’s final wave hit in early 1919 and ran through spring, the CDC says. By summer, the pandemic had waned, although, Short says, the virus continued to be seen through the 1920s.
The Nevada State Museum exhibition will run through late April. Despite all of the advances in medicine since then, there’s really nothing to prevent a similar pandemic today, Short says.
We now know that the virus that caused the pandemic “was a variant of the H1N1 strain, which is what we see every year,” Short says. “Some people say it’s only a matter of time before we have a mutation like this one.”
Yes, it could happen again
According to the Centers for Disease Control and Prevention, a pandemic occurs when new influenza viruses emerge that “are able to infect people easily and spread from person to person in an efficient and sustained way.”
The agency identifies four influenza pandemics over the past century — in 1918, 1957, 1968 and 2009 — with the 1918 pandemic as the most severe.
Can a pandemic like the 1918 event occur again? Sure, said Dr. Joseph Iser, chief health officer of the Southern Nevada Health District.
“Scientists are always looking around the world for new strains of influenza,” he said, with an eye toward determining those that might change in ways that affect humans.
But with the vast array of strains that are out there or may emerge, it’s likely, Dr. Iser says, that “there will be another pandemic.”
Which makes now a good time to underscore the need to follow basic flu prevention practices long before whatever might arrive does arrive.
First, get an annual flu shot.
It’s true that “not all influenza vaccines are equally effective from year to year,” Iser says. That’s because flu vaccines are produced several months in advance based on predictions of which flu strains are likely to be circulating.
But even a less-than-perfect match still will help to reduce the chances of catching the flu and, if a bout of flu does come, may make it less severe and of shorter duration.
Many people “still have an inappropriate fear of vaccines,” Iser adds, but there’s “just no evidence of any of the (negative) claims people make related to vaccines.”
Employ basic hygiene practices, including frequent handwashing, particularly after touching such potentially infected surfaces as doorknobs. The flu virus “doesn’t live that long,” Iser says, but it can live for a few hours on surfaces.
Avoid touching your eyes, nose or mouth. Those are the easiest routes by which viruses are transmitted.
Sneeze or cough into the crook of your clothed arm. “Try not to use napkins or handkerchiefs or Kleenex because it generally soaks through,” he says.
Take care of yourself generally. Get plenty of rest, stay hydrated, eat nutritiously and exercise regularly because “it boosts your immune system,” Iser says. “Do the sorts of things your mother used to tell you to do.”
Finally, “if you are sick, don’t go to school, don’t go to work.”
Pandemic time line
Here, from the Centers for Disease Control and Prevention, are some key events of the 1918 influenza pandemic.
April 1917: The United States enters World War I.
March 1918: Outbreaks of flulike illness are reported in the U.S., and more than 100 soldiers at an Army camp in Kansas are stricken.
April 1918: The first mention of influenza — about 18 severe cases and three deaths in Kansas — appears in a weekly public health report.
September 1918: A second wave of flu hits an Army training camp and a Navy facility in Boston. The second flu wave peaks between September and November, and causes most of the pandemic’s deaths.
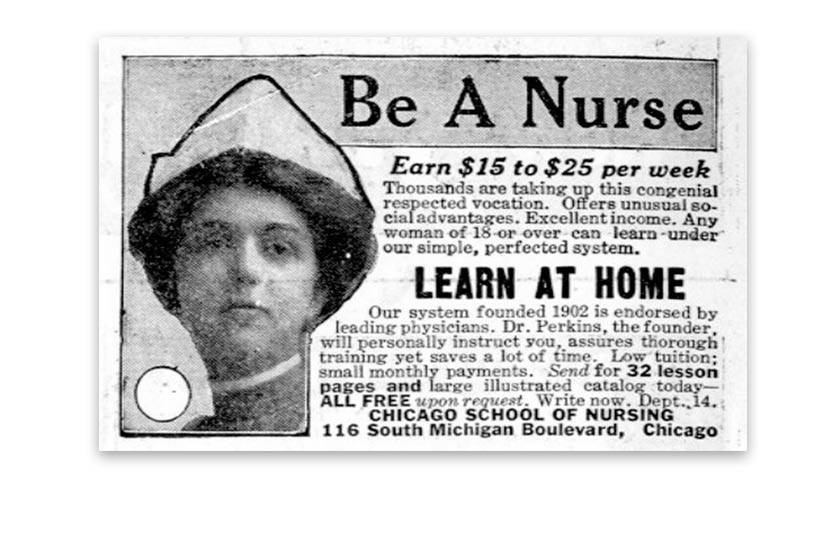
October 1918: The pandemic kills about 195,000 Americans during this single month. The U.S. experiences a severe shortage of nurses — due to both military deployment of nurses and not employing trained African-American nurses. In hard-hit Philadelphia, cold storage plants are used as temporary morgues and a trolley car manufacturer donates 200 packing crates that are used as coffins.
November 1918: World War I ends.
January 1919: The pandemic’s third wave hits in the winter and spring, killing more before it finally wanes in the summer. According to the CDC, the number of civilian and military deaths during the pandemic surpassed the number of deaths resulting from World War I.
Related
Taught by tragedy, Las Vegas mom now a stickler for flu vaccinations
Contact John Przybys at jprzybys @reviewjournal.com or 702-383-0280. Follow @JJPrzybys on Twitter.



















