Stepping in to slow macular degeneration



The waitress stops by the table where Linda Higgins is finishing a slice of pizza to drop off the bill. Higgins closes one eye and squints to scrutinize the bill and, later, when the waitress returns with a credit card receipt, to make sure she’s signing in the right place.
It’s just one of the many adjustments – large and small – the 57-year-old Las Vegas resident has had to make since being diagnosed four years ago with macular degeneration, a disease that results in serious vision impairment.
Macular degeneration is a huge problem, according to Dr. Kwang Lee of the Nevada Retina Center in northwest Las Vegas. About 15 million North Americans have been diagnosed with some form of macular degeneration, he notes. And that number is expected to rise significantly as baby boomers grow older, because age is a major risk factor for the eye disease.
About 3.9 percent of Americans between the ages of 50 to 59 have intermediate or advanced age-related macular degeneration, according to Macular Degeneration Research, a program of the American Health Assistance Foundation. That percentage jumps to 14.4 percent for ages 70 to 79.
"The magnitude of the problem is tremendous," Lee says. "As baby boomers age, we’re going to have more people diagnosed with it."
There are two forms of macular degeneration: wet and dry. Dry macular degeneration occurs when the light-sensitive cells of the macula slowly break down. Wet macular degeneration occurs when blood vessels behind the retina leak, impairing vision.
About 80 percent to 90 percent of age-related macular degeneration is the dry type, which progresses gradually and slowly. But about 10 to 20 percent develop the other type.
There is no cure, but it can be treated to slow its progression.
Among other risk factors for macular degeneration are genetics, light skin and eye color, obesity, hypertension, high cholesterol and smoking.
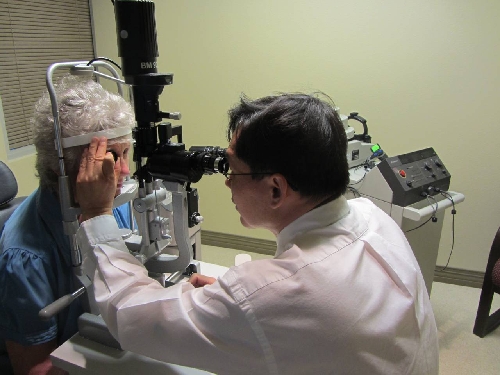
"Early intervention can sometimes help minimize vision loss," says Lee, who is Higgins’ doctor but notes because of privacy regulations he cannot speak specifically about her case.
Lee recommends that people have regular eye dilations, which can reveal evidence of the disease.
"I think it’s a good idea," Lee says. "Regular eye dilation examinations are how you diagnose macular degeneration."
An Amsler grid also can help reveal problems, he adds. The patient covers one eye at a time while looking at the grid. This can reveal an area of distortion and/or a blind spot.
Higgins says she has the wet form in one eye and the dry form in the other. She notes her elderly mother has the dry form of the disease.
Higgins maintains a strong positive attitude about having the disease but remains upset with an earlier ophthalmologist’s handling of her case.
"It was really unfortunate for me because the eye doctor that I was going to kept saying: ‘Oh, let’s just wait and see. Let’s just wait and see.’ But I started noticing that if I was looking at a line of text, all of a sudden it would start dipping down and coming back up again. And that’s how it first started happening."
Initially, Higgins thought the printer was off-kilter, but then she started noticing it happening all the time. So she returned to the eye doctor, who conducted a dye test that showed where blood vessels behind her retina had broken, leaving pools of fluid that were affecting her vision. Over a two-year period, Higgins had been given the dye test three times, but the doctor never recommended she see a specialist until she got angry one day in his office.
"I’m trusting him, and he just kept saying, ‘Let’s just wait and see.’ So finally I was hysterical in the office, saying: ‘I can’t see and you’re just telling me wait. Wait for what, until I’m blind?’ ” she recalls. Finally the doctor said he would recommend a specialist. Higgins called the Nevada Retina Center and was asked when she could come in. "And I said, ‘I don’t know, maybe next week,’ and they said, ‘No, now.’ "
She immediately went to the center, and that’s when she learned she had wet macular degeneration in one eye and the dry form in the other. All wet macular degeneration starts with the dry form, but the dry form doesn’t always progress to the wet form.
"I was so upset with that guy," she says, declining to name the other doctor. Higgins says she believes if she had been sent to a specialist sooner she would have suffered less vision loss because treatment to stop the progression of the disease would have been provided sooner.
Now, she goes to the Nevada Retina Center once a month to receive an injection of medication in the eye with wet macular degeneration. The shot contains a drug that can help control the abnormal blood vessel growth and stabilize or, in some cases, improve vision.
It’s an ordeal that once a year requires being cleared by doctors, who check her carotid artery to make sure she would not have a stroke or heart attack, a regimen of antibacterial drops, dilations and eye tests, and then the eye is numbed before the doctor proceeds with the injection.
Her husband, Chris Stanley, accompanies her to the appointments.
"If she’s going to go through this thing, I’m going to be there myself," he says. "She handles the whole procedure better than I do. I don’t watch that."
Higgins experienced pain the first time, but once she and the doctor dialed in the perfect amount of time to let the numbing medication take effect, she now feels no pain, she notes.
"But what does happen, sometimes after the shot, I lose complete vision, it goes completely black. You have to wait until your pressure comes back. I’ll start seeing shadows and stuff, and it comes back, and them I’m like, ‘Oh I can see.’ "
The injections do not come cheap, costing some $2,600 per shot, plus $600 per doctor visit. Insurance covers some of the cost, but she is left with a bill of $564 a month.
"I can’t do that," she says. "Thank God my doctor recommended me for something called the Chronic Disease Fund."
The fund, made possible by donations, pays a portion of her cost and makes the care affordable.
That cost may become even more affordable if research into a new type of injection may allow a more time-released dose, making each injection last longer.
"Instead of going every month for your shot, it’ll be time-released so you can get a shot, and it might be every three months."
Stanley says his wife was initially very distraught by the diagnosis, but has adjusted well.
"Yes, she’s unhappy she has it, yet it has not dampened her personality (nor has she) let it control her life," he says. "Linda really tries to keep a good attitude and I think that really helps a lot."
There are issues, such as inability to read small writing and misjudging depth perception.
When they’re out to eat, Stanley often has to pull out his iPhone to light the menu for Higgins or read items for her. He’ll also guide her as they approach a curb or another potential hazard. At home, Stanley purchased a larger television with an extra-sharp picture to ensure Higgins could enjoy her favorite programs, including Saturday cooking shows. Higgins also uses magnifiers to help with reading.
Stanley worries how Higgins will adjust when she is no longer able to do her hobbies, such as make jewelry, write and illustrate children’s books, or design cards and buttons.
"It’s getting harder for her. Trying to thread something through when you have only one good eye," Stanley says. "She still does it, but I know it takes longer for her to do."
She can still drive herself to work, which is just four miles from home, and to other locations. She also remains productive in her job as a legal secretary, but it has its challenges because her position requires a lot of reading.
She praises her employer, the law firm of Lee Hernandez, Landrum, Garafalo and Lee, which allows her to use a large 24-inch monitor to do her work and gives her plenty of leeway for her appointments.
"Everybody’s been fantastic," she says.
Higgins is effusive in her praise for the treatment she is receiving from Lee.
"I love him. He’s wonderful," she says. "He makes it not a horrible experience."
While Higgins maintains her upbeat attitude, thinking about the future can bring on anxiety.
"What scares me is that I don’t know when this (pointing to her eye with dry macular degeneration) is going to switch from dry to wet," she says. "Because once that happens I’m done. I won’t be able to drive. I won’t be able to work. I am an artist. I won’t be able to do any of that stuff. It’s unfortunate, but what are you going to do, right? I mean, everybody’s got something."
That said, Higgins notes she also is a firm believer in technology.
"I am hopeful that at some point while I am still alive they will come up with something that will help this," she says. "And I ask my doctor all the time, ‘If you need me to be like a test subject, I’ll do it.’ "


















