Some parents at odds with experts about sharing beds with infants





She has seen weeping parents sit with their dead baby in the emergency room for hours, taking turns holding their precious child, pleading for God to make an awful accident just a bad dream.
Sometimes they whisper. Sometimes they wail. Sometimes they sing their little one’s favorite song.
“It is way beyond tragic, way beyond sad,” nurse Nancy Harpin said Thursday outside the pediatric emergency room at University Medical Center. “When we see that there are no signs of abuse, that it was a terrible accident, we allow parents as much time with the child as they need. Losing a child this way is so horrific, has such a lasting effect, that you want to help them all you can.”
An infant with no health problems. Loving parents with the best of the intentions. Then, often in the wee hours of the morning, parents wake up to find their child is not breathing, a tiny, helpless victim of an unsafe sleeping environment.
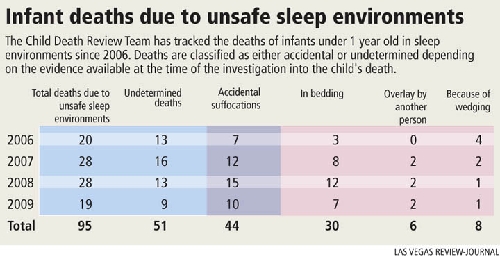
From 2006 to 2009 in Clark County, 95 babies less than 12 months old died because bedding or stuffed animals or pillows or sofa cushions or a soft bed or a wall didn’t allow them to breathe. Or their necks weren’t strong enough to lift their heads and they suffocated lying face down in the crib. Or mom or dad or a sister or brother or family friend rolled over on them in their sleep.
“We need to find a way to decrease these deaths,” said Dr. Andrew Eisen, chairman of the Clark County Child Death Review Team, which meets monthly to assess and analyze cases involving the death of any child under 18. “We keep seeing this kind of thing over and over again. The numbers are alarming.”
Over that same four-year period, there were 41 accidental drownings involving children, and 83 deaths in motor vehicle accidents. One child died from exposure in an overheated car.
Tara Phebus, a research analyst for the Nevada Institute for Children’s Research and Policy, which keeps statistics for the review team, said the county didn’t begin tracking children’s deaths from unsafe sleeping conditions until 2006.
The statistics have shaken Gwen Osburn, who heads the Southern Nevada Health District’s Nurse-Family Partnership program for first-time mothers.
“We definitely have some education to do,” she said. “These are senseless deaths.”
A national study between 1984 and 2004 found infant death rates attributed to strangulation or suffocation in bed jumped fourfold, from 2.8 deaths to 12.5 deaths per 100,000 live births.
In its wake, the American Academy of Pediatrics issued a statement in 2005 on safe sleeping practices, including a recommendation that has become highly controversial: Infants should not share a bed during sleep.
“Each child deserves his or her own safe sleeping space,” Eisen said, echoing what has become the dominant public health position in the United States. “We’re in favor of a crib or bassinet for the newborn, one with a firm mattress and without soft objects and loose bedding, close to the parents’ bed.”
That position, while understood to be well-meaning by everyone in the child-care community, is seen by some as unnecessarily narrow, a harsh rejection of behavior practiced by many parents and children since the beginning of humankind.
“I do believe you can sleep safely next to your child,” said Mandie Medford, who last week displayed how she uses a small boxlike compartment in her northwest Las Vegas home to hold 2-month-old Grace between her and her husband, Larry, a science teacher at Rogich Junior High.
“There’s no way covers can go over her because she’s on top of the comforter. It makes it so much easier for me to breast feed and bond with her. Bonding is so important.”
The Medfords are confident the compartment that Grace sleeps in helps her safely maintain her sleep position, but public health officials say such devices haven’t been tested enough to show safety.
Lisa Stark and her husband, Brent, a Southwest Airlines pilot, also wanted to sleep with their newborn to help them bond as a family.
But as they sat in their Henderson home last week, Brent explained why they had to move 6-week-old Sam to a bassinet next to the bed.
“I couldn’t sleep because I was afraid I would roll over on my son. I couldn’t stop thinking about it. And there was no way I could fly with no sleep.”
Although the question of bed sharing continues to create debate, other public health recommendations regarding safe sleep for infants receive almost uniform backing, regardless of whether individuals believe bed sharing can be done safely.
Those recommendations include:
■ Infants should sleep on their back on firm and clean surfaces, in the absence of smoke, and their heads should never be covered.
■ No stuffed animals or pillows should be around the infant, and the child never should be placed to sleep on top of a pillow.
■ If blankets are used, they should be tucked in around the crib mattress so the infant’s face is less likely to become covered by bedding.
■ Bean bag, water bed and mattresses made of fluffy material such as sheepskin that cause a sleeper to sink should not be used. Mattresses should tightly intersect the bed frame.
■ Infants should never sleep on couches or sofas, with or without adults, where they can slip face first into a crevice or get wedged against the back of a couch.
James McKenna, a professor of biological anthropology at Notre Dame University, has long been an advocate of safe bed-sharing for breast-feeding mothers. A breast-feeding child naturally needs the mother as close as possible, he said. But McKenna stresses strict guidelines for bed sharing.
Persons on sedatives, medications or drugs, or who have been drinking, should not sleep with an infant, McKenna said.
And he said extremely obese persons, who may not feel where their infant is, should not sleep on the same surface as a child. Nor should an infant ever be in bed with siblings, who he said are unable to control how they sleep.
He also believes that the bed frame should be removed and the box spring and mattress moved to the center of a bedroom. The child should sleep under the mother’s arm, near her breast.
“I don’t think women who bottle feed should co-sleep with a child, because so often the infant is put on top of a pillow for feeding,” McKenna said.
Dr. Fern Hauck, a University of Virginia researcher who was on the American Academy of Pediatrics task force that made the 2005 recommendation against bed sharing, said the guideline supported by the academy is based on the best research studies available. She said even more research must be done on safety.
She acknowledges what McKenna says is true, that studies have shown that breast-feeding helps decrease the risk of Sudden Infant Death Syndrome, but Hauck does not believe that means the child must sleep on the same surface as the mother.
She said it is unlikely that bed sharing can be made truly safe because few parents are going to largely do away with blankets and pillows that put babies at risk.
“You must remember that all of us on the task force are breast-feeding advocates,” she said. “We tried to be objective as possible.”
How many people, she wondered, can realistically be expected to do as McKenna suggests and place their bed in the middle of a room without a frame.
And the rollover risk is always there, she said.
Hauck participated in a safe sleep summit that the Milwaukee Health Department held earlier this year. Experts discussed how schools, hospitals, community groups and social agencies could work together on the issue.
Anna Benton, director of family and community health services for Milwaukee, said city officials became alarmed at the number of unsafe sleep deaths for infants there, about 90 over a four-year period.
“We felt we had to do a public service campaign,” she said.
Because the campaign, which includes a strong media effort, is so new, Benton said it is unknown whether it is effective.
One poster and commercial in the campaign show the headboard of an adult bed as a tombstone with this inscription: “FOR TOO MANY BABIES LAST YEAR, THIS WAS THEIR FINAL RESTING PLACE.”
That kind of tactic hurts public health efforts, McKenna said.
“Scare tactics, where people are basically accused of criminal behavior, aren’t going to work,” he said. “People just tune you out because they’re well aware that public health messages tend to change. Parents are doing their best.”
Hauck said she understands Americans say they are confused by a public health establishment that often changes its message.
She said Dr. Benjamin Spock, who was known as the nation’s baby doctor, advocated during the 1950s that babies should sleep on their stomachs. Before that, doctors had largely recommended that they sleep on their backs.
Then in the 1990s, the American Academy of Pediatrics again said it was safer for infants to be put on their backs to sleep.
Hauck said studies found that the move to infants sleeping on their backs cut sudden infant deaths in half.
The reason why sleeping on the back is so much safer is not entirely clear, researchers say. But it may be related to findings that suggest that an infant who sleeps on their stomach gets less oxygen or gets rid of carbon dioxide less because of rebreathing the air from a pocket of bedding pulled up around their noses.
“I do wish the medical community would come together with one voice on this issue of safe sleep,” Hauck said. “We should get our act together, because what is at stake is so important.”
Las Vegas hospitals are trying to educate new mothers and families on safe sleeping for infants.
Last Thursday, a day after Teiana Causey gave birth to 7-pound, 14-ounce Adam Causey at UMC, she and her husband, Adam Sr., listened to registered nurse Dawn Lipkin share the safe-sleep measures favored by public health officials.
Though Teiana and Adam Causey slept with 3-year-old daughter Taylor after she was born, they don’t plan on doing the same with their son.
“We’re going to be as safe as we can,” Teiana Causey said.
The Clark County Child Death Review Team, which has 19 members drawn largely from public health, public safety and university disciplines, has a sense of urgency toward getting a safety message out to new parents.
“We need to put an end to this kind of tragedy,” said Paula Hammack, a death review team member and assistant director for the Clark County Department of Family Services. “There’s no reason for this to go on.”
Another team member, Dr. Alane Olson, a medical examiner with the Clark County Coroner’s office, said it is frustrating to see children die because they don’t have a safe place to sleep.
“We keep seeing the same kind of scenarios. A child dying face down in a pillow or a fluffy comforter or in a crowded bed or crib. A bassinet or crib isn’t a storage place for diapers or clothes. And then the grief associated with this is just horrible for the parents. The word has to get out. Pediatricians have to speak with one voice. A child must have his own bed. In a free-for-all in bed, the child is going to lose.”
The health district’s Gwen Osburn said she is hopeful that a grant request she has written for a major public service campaign for Clark County on safe sleep for infants gets funded after the first of the new year.
UMC nurse Nancy Harpin doesn’t want to see any more babies coming to the hospital by ambulance because of unsafe sleeping situations. And yet she fears she will.
“Because of the economic problems we’re having right now, we are having more and more medical problems created because so many people are sleeping in one bed.”
Harpin has studied the research on parents who lose children through sleeping accidents and found that more than 80 percent of the parents divorce. One parent often blames the other.
The horror of finding your suffocated child’s body leaves parents trapped inside a legacy of guilt and grief for the rest of their lives, she said. Day after day they must move amid their shattered dreams, the promise of what might have been, what should have been.
What takes the child’s life is an accident, she said, but still the parent feels the burden of a life sentence for which there is no parole.
Contact reporter Paul Harasim at
pharasim@reviewjournal.com or 702-387-2908.












