There may never have been another point — at least in our lifetimes — when the work, sacrifices and impact of nurses, and other health care workers, were more obvious to so many people than now.
Those working on the front lines of the coronavirus pandemic are among the most visible heroes of this often-frightening era. But nurses have been making our lives better since long before this crisis, and their impact is felt far beyond hospitals and nursing homes. Nurses give us care and comfort at every phase of our lives: from the womb to the tomb, as they say (and as we see below, sometimes before we are even conceived).
Since Wednesday is National Nurses Day, we honor here just a few of the more than 47,000 licensed nurses in Nevada who make Las Vegas a better place to live, day in and day out, year after year.
Nurses are there when the last breath is taken and nurses are there when the first breath is taken
Christine Bell

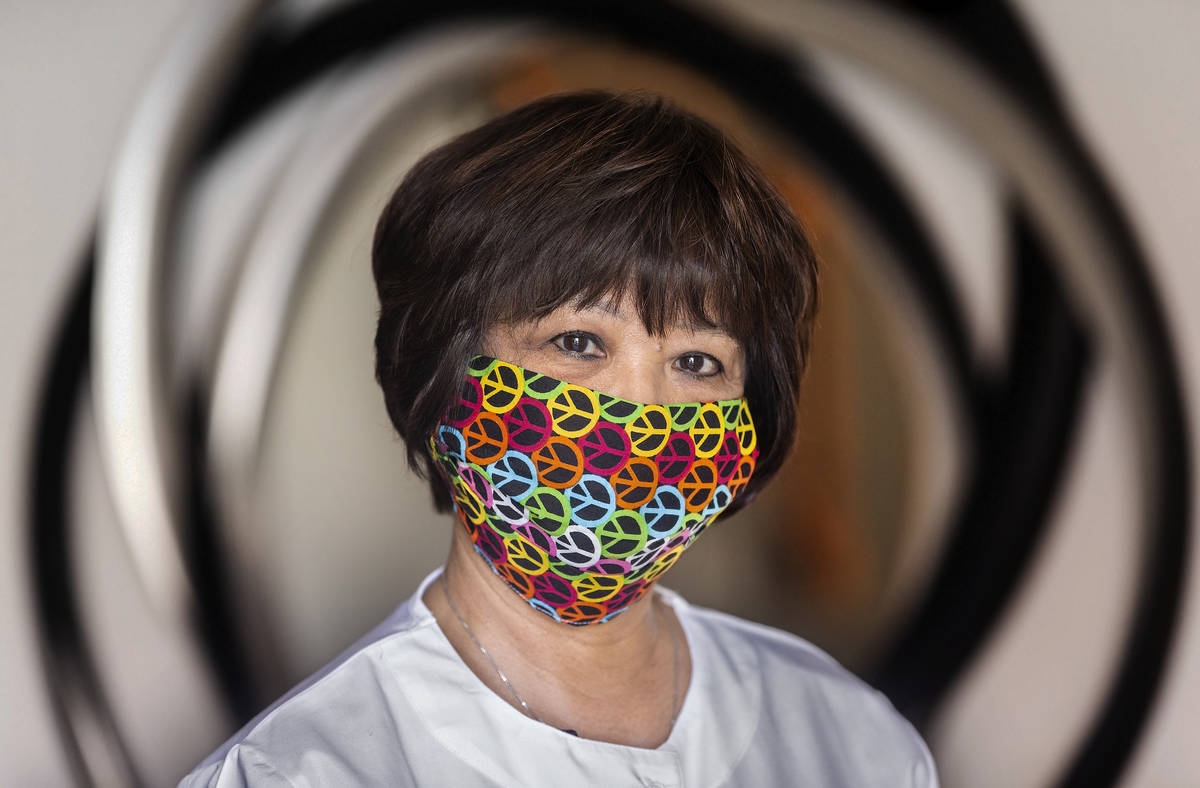
Nita Peterson
Nurse, Sunset Surgery Center and Red Rock Fertility
Before attending nursing school, Nita Peterson worked as a medical assistant, and had two degrees under her belt. None of that, she says, compared to the challenges and rewards of nursing.
“I have an associate’s degree. I have a bachelor’s degree in business management. And then my nursing degree. And out of all of it, my nursing degree was probably the hardest, but the most rewarding.”
Don’t get me wrong, I loved hospice. But just to start at the beginning of life was so rewarding. And it felt so good to see some of these people so happy … that I just decided that that’s where I wanted to be
Nita Peterson
In the five years she’s been a nurse, Peterson has worked in several areas, including hospitals and hospice, before deciding to work in the fertility field.
“Don’t get me wrong, I loved hospice. But just to start at the beginning of life was so rewarding. And it felt so good to see some of these people so happy … that I just decided that that’s where I wanted to be.”
In her current job, she often can help patients before their treatment begins by reassuring them.
“Some have been trying to (conceive) for a long time. Some of them cannot understand why it’s easy for others and so hard for them. I’m able to relax them and let them know they’re not alone.”
The big payout, of course, comes when they’re successful in their efforts.
“To know that they’ve conceived at our facility … that makes my day.”

Digna James
Weekend night charge nurse, UMC Trauma Center
“I always wanted to do something in medicine, and nursing just drew me,” Digna James says.
James, who received her bachelor’s degree from UNLV in 2001, has lived in Las Vegas on and off since 1994. And while she temporarily relocated when her husband’s 20-year military career took them elsewhere, she says, “most of my family is still in Vegas. This is still considered home.”
I always wanted to do something in medicine, and nursing just drew me
Digna James
Her interest in nursing dates back to her high school years in Reno, where she participated in some programs introducing her to the field.
“I think I was always meant to take care of people.”
Like many medical professionals, James has seen her working conditions drastically change in the face of COVID-19. For her, the most difficult part is having to wear a mask at all times.
“A lot of us feel that we’re losing something, because now we have covered faces (when we’re with) patients. Whereas before they could see a smile, and we could try somehow to make them feel better, now we’re covered up — for everyone’s protection.”


Dave Tyrell
Clinical manager, UMC’s Center for Transplantation
The son of a nurse, Dave Tyrell spent 20 years working in warehouse distribution, climbing to an assistant vice president position at T.J. Maxx and Marshalls’ parent company Marmaxx, before “going through kind of a burnout and realizing I had not pursued what my life’s dream was.”
So at age 41, he went back to school for nursing at UNLV.
But the day I made the decision to go to nursing school, I was absolutely sure that this is what I was meant to do, this is what I needed to do
Dave Tyrell
“It was a hard decision,” he says of the career change. “But the day I made the decision to go to nursing school, I was absolutely sure that this is what I was meant to do, this is what I needed to do.”
Tyrell enjoys working with transplant patients because it allows him to follow their progress over an extended period of time, from their referral until up to a year after their surgery.
“They come in very sick. And then you take them through the kidney transplant process, and they’re like a totally changed person. And that’s why I love the transplant area so much.”


Audra Sommes
School nurse, CCSD (Leavitt Middle School, Dean Allen Elementary and Brinley Middle School)
After serving as emergency room director at Summerlin Hospital, Audra Sommes was working as a charge nurse in Sunrise Hospital’s pediatric emergency room when she adopted her daughter from China in 2004. That love of children led to her first school nurse position in 2011, at what was then Andre Agassi College Preparatory Academy.
We don’t put on Band-Aids all day long
Audra Sommes
Sommes wants people to know that school nursing isn’t what many expect.
“We don’t put on Band-Aids all day long,” she explains. “That’s not what school nurses do. It’s much more assessment.”
Sommes recounts the story of a student she referred to a clinic after noticing some troubling symptoms that his parents had dismissed as simply clumsiness.
“When I sent him over to the genetic clinic, it turned out he had a very rare genetic disease that was life-threatening.”
That work has become more challenging with schools closed because of COVID-19. But she’s still trying to remain in touch with students and their families, through text messages and video calls.
Sommes also volunteers at the Cashman Center homeless shelter, where they are caring for and quarantining those with COVID-19.
“I’m able to use my nursing skills differently (there),” Sommes says of caring for patients at their bedside again.

Angela Collins
Chief nursing officer at Nathan Adelson Hospice
“Not all nurses wear scrubs.”
During her 20-year career, Angela Collins has spent plenty of time in the traditional nurse’s garb while working in hospitals. These days, however, she’s “the nurse that wears business attire.”
Though she estimates 90 percent of her work now is administrative, she still takes time to meet with hospice patients receiving end-of-life care and their families.
I think we really help add quality to people’s lives. We never want anyone to die alone, in pain or afraid
Angela Collins
“I do rounds in our units rather routinely — a little less right now with COVID,” she says. “But I do rounds, and get out in the field, sometimes with our nurses, just to meet the families and see how things are going.”
Collins knew she wanted to be a nurse when she was in eighth grade. She got into hospice work about a decade ago, joining Nathan Adelson Hospice last September.
“I never thought I would do hospice,” Collins says, “but it’s one of the most truly rewarding forms of nursing that I’ve ever been a part of.”
While hospice patients and their families know that they won’t recover from their illnesses, Collins says that the care her staff provides is incredibly important.
“I think we really help add quality to people’s lives. We never want anyone to die alone, in pain or afraid.”


Clare Gierth
Care coordinator, Cleveland Clinic Lou Ruvo Center for Brain Health
Clare Gierth began working at the Cleveland Clinic in Cleveland in July 2010, transferring to Las Vegas in 2013. As a care coordinator on the cognitive disorders team, she works with Alzheimer’s and dementia patients. Her duties include offering guidance and advice on each patient’s condition and helping them find the support they may need.
I didn’t expect … to actually form such close bonds with the patients and their families
Clare Gierth
Much of the work is done virtually, with patients around the globe. And her relationships with those patients are long term.
“When we get a patient with dementia, there’s no cure,” she explains. “So as long as they’re coming to the Cleveland Clinic, I’m their go-to. I’m with them for the rest of their life.”
Gierth says those relationships are the most rewarding part of the job.
“I didn’t expect … to actually form such close bonds with the patients and their families. Even when it comes time for the end of life, the patient’s family still calls up and talks to me and tells me about it,” Gierth says. “I was surprised (to) find myself getting teary — (because) I really did help, and they’ve had an impact on me.”


Alona Angosta
Associate Professor/Director of the Family Nurse Practitioner master’s degree program, UNLV.
When Alona Angosta taught undergraduate nursing courses at UNLV, she always asked her first-year students what brought them to nursing. It’s a question she has no difficulty answering.
“I chose nursing because of my love for science, teaching, caring, helping, serving and advocating for others who are in their most vulnerable situations,” Angosta says. “I can’t think of any other profession that provides the holistic care approach and opportunity to emphasize these attributes to help improve patients’ lives.”
I chose nursing because of my love for science, teaching, caring, helping, serving and advocating for others who are in their most vulnerable situations
Alona Angosta
Born in the Philippines, she moved to the U.S. in her early teens, when her father retired from the Air Force. In addition to her teaching and research work at UNLV, she’s a board-certified nurse practitioner who works at a clinic in Henderson. Angosta also is a board member of the National Coalition of Ethnic Minority Nurse Associations and is the recipient of the NP Advocate State for Excellence award by the American Association of Nurse Practitioners. But educating the next generation of nurses, she says, provides rewards unlike those attained from her other roles.
“As a teacher, the rewarding moment would be when you see your student graduate and is now a nurse making a difference in the community.”


Carlos Esparza
Emergency room nurse practitioner and chief clinical officer for OptimuMedicine
Carlos Esparza’s career has included time in a local trauma intensive care unit and two years as a medical flight nurse, transporting patients by air in Las Vegas and Elko. Today he works full time as an emergency room nurse and does home visits for a friend’s clinics. He’s also a partner in the medical transport company OptimuMedicine, which owns three ambulances and offers air transportation for patients.
“I do the education and the training,” he says of his role at OptimuMedicine. “I (also) do transports here and there.”
I was not the only one who got sick. There were several other people who did, that I know of, and we were scared for some of them
Carlos Esparza
All of those jobs have changed “tremendously” since the COVID-19 outbreak, Esparza says — especially after he was diagnosed with the virus and “down for two straight weeks.” While that experience allows him to relate better to patients who have the virus, or are afraid they may have it, he says the experience has brought everyone in his field much closer together.
“I was not the only one who got sick. There were several other people who did, that I know of, and we were scared for some of them.”
Fortunately, Esparza and his colleagues all have recovered and been cleared to return to work. Nonetheless, he says, having the illness has changed them.
“We’re closer with everybody and we appreciate each other more.”
Doris Bauer
Director of nursing, Sisu HealthCare Solutions
Bauer graduated nursing school in her native Philippines before moving to the U.S. in 1978. While she has experience in critical care, neurological nursing, orthopedic nursing and medical surgical nursing, she has been working as an infusion nurse since moving to Las Vegas in 1994. As manager of Sisu HealthCare Solutions’ offices in Las Vegas and Arizona, she oversees a team of nurses that provides long-term, home-based intravenous therapies.
“We teach the patients and their families to become independent with the IV therapy they’re given in the hospital, in their home,” Bauer explains. “It’s a different niche. When you go into the home arena, you have difference stresses, and it takes a special kind of nurse to work in that situation.”
We teach the patients and their families to become independent with the IV therapy they’re given in the hospital, in their home
Doris Bauer
Bauer and her team often encounter patients who are completely on their own and in need of more than medical care. She’s found herself picking up groceries for a patient or even collecting funds to cover drug costs.
Bauer also is active in the local Filipino community. She’s in her second term as president of the Philippine Nurses Association of Nevada and hosts the PHLV radio podcast “Filipinars.” Her work in response to COVID-19 has included organizing food drives for furloughed workers and making masks for people on the front lines of the fight.


Denise Horvath
Nurse practitioner, Comprehensive Cancer Centers of Nevada
Horvath was 19 years old, in her second year at New York University on a pre-med scholarship, when she realized “even with my hardest work, I was not going to be at the top of my class.”
Instead of pushing ahead with plans to become a doctor, the daughter of a nurse and a police officer decided to give nursing a try.
Honestly, after the first day of clinical for nursing, I thought, ‘Thank God this happened!’
Denise Horvath
She hasn’t looked back.
“Honestly, after the first day of clinical for nursing, I thought, ‘Thank God this happened!’ I was so happy. I loved nursing.”
After graduating in 1995, she returned briefly to Las Vegas before joining the Peace Corps, where she was assigned to a girls school in Nepal. There, she taught first aid and community nursing to girls whose acceptance to school had rescued them from being sold into the sex trade.
“They were just so wonderful and happy, she says of her students. “I knew most of them didn’t have enough food. They didn’t have clean clothes. But every day they were there and they just wanted to learn.”
After contracting dysentery and mononucleosis, Horvath returned to Las Vegas early. Her local career included time at Valley Hospital, 10 years at UMC Trauma and 14 years as a flight nurse before she took her current position in the lung center at Comprehensive Cancer Centers of Nevada. Working in a hospital setting, with pulmonary patients, she’s seen a lot of COVID-19 patients. But she believes her training has prepared her to deal with it.
“It’s a stressful job,” Horvath says. “But I see it as, this is the kind of stress I was made for.”















