With Nevada hospitals short on beds, leaders plan for the ‘unthinkable’
A rapid influx of coronavirus patients could soon inundate Nevada hospitals, pushing them past their capacity and threatening health care workers’ safety.
For every 17 people likely to be hospitalized by COVID-19, the state has only one staffed bed at its short-term acute care and critical access hospitals, according to a Review-Journal data analysis. The vast majority of these beds are already occupied as part of hospitals’ normal operations, making availability even more scarce.
Facing a potential crisis, local health officials say all Nevadans must employ strategies like social distancing and self-isolation to slow the spread of the respiratory illness.
“This is an unprecedented situation. We don’t know what it’s going to look like,” said Dr. Joe Corcoran, the chief medical officer overseeing HCA Healthcare hospitals in Nevada and California. “We’ve challenged our facility leaders to plan for the unthinkable.”
The number of confirmed cases of COVID-19 across the U.S. has exploded in recent days. In Nevada, the number increased nearly sixfold to 154 in the past week. The Southern Nevada Health District reported Friday that patients in almost 16 percent of its 126 cases had been hospitalized.
The rapid spread of the disease has stoked concerns not only about overcrowded hospitals but also about an overwhelming demand on health care essentials like protective equipment, ventilators and even front-line personnel.
Overseas, COVID-19 has pushed northern Italy’s health care system to its breaking point in a matter of weeks. The disease had killed more than 4,000 people in the country as of Friday, and some hospitals have reportedly resorted to caring only for patients most likely to recover.
In Las Vegas, operators of the largest hospitals say what happens next will be pivotal. They’ve already begun to take extraordinary measures to prepare, such as closing their doors to nearly all visitors and creating new, COVID-19-specific isolation wards.
“We’re right at that point where in the next week or two we’ll see what trajectory we’re taking,” said Dan McBride, regional chief medical officer for the Valley Health System. “We could follow a trajectory that is similar to Italy, but we’re not certain that’s going to occur.”
Gov. Steve Sisolak on Friday warned that Nevada’s hospitals were facing a potential “tsunami” of COVID-19 cases. He issued a mandatory shutdown of most nonessential businesses in the state to help curb the spread of the coronavirus.
“If we do not do everything we can to slow this virus, hospital beds will soon be completely filled with COVID-19 patients,” he said at a news conference. “There will be no beds to set broken bones, treat heart attacks or use for other necessary medical procedures.”
Hospital bed numbers
Nevada has about 5,500 staffed hospital beds spread across its short-term acute care and critical access hospitals, according to the Nevada Hospital Association. Those facilities have about 760 rooms in intensive care units, designated for the most seriously ill or injured patients.
But the vast majority of the facilities’ beds, about 83 percent, were already occupied as of Friday, the NHA reports. ICU rooms were about 85 percent occupied.
A model published by the Harvard Global Health Institute on Tuesday estimated at least a fifth of American adults would contract COVID-19. Less than one-third of the infected would need to be hospitalized, and about 5 percent of the infected would require intensive-care treatment.
In Nevada, that translates to nearly 94,000 hospitalized adults in a best-case scenario. Almost 19,000 of those would need intensive-care treatment.
Those numbers dwarf the bed capacity reported by the Nevada Hospital Association, and the gulf is far greater when taking into account hospitals’ current occupancy. And it’s why health officials have been preaching “flattening the curve,” or keeping the spread of the disease at a manageable level.
“The whole point is to try to keep it so (that) even if we have the same number of patients overall, they’re not getting sick and hitting the hospitals all at the same time,” said Christopher Lake, the Nevada Hospital Association’s executive director of community resilience. “Theoretically, you treat a patient and they get discharged, so that bed is available for the next person that gets sick.”
Las Vegas Valley hospitals report that they have already spent weeks preparing for their capacity to be strained.
Some hospital systems are rescheduling nonessential surgeries to lower their number of in-patients. University Medical Center is improving its telemedicine capabilities to lower the number of people who come to the hospital for evaluation, including for COVID-19.
“The idea is to maximize the resources we have and minimize the number of patients who are not very sick that come to our hospital,” said Dr. Shadaba Asad, the hospital’s medical director of infectious disease. “For the vast majority of the public, this will be a mild respiratory illness, so if you stay at home, you will get better. You do not need to come to the emergency room.”
Still, a surge is anticipated.
HCA Healthcare’s Corcoran said the company’s three local hospitals have created plans to add as many as 100 intensive-care beds should the need arise.
UMC is instead looking at how to maximize its current capacity. That includes placing multiple patients infected with COVID-19 in the same room and moving patients out of intensive-care beds when possible, Asad said.
Personal protective equipment
But beds are not the only shortage hospital operators and health officials are concerned about.
Personal protective equipment such as face masks, gloves, goggles and gowns is in widespread demand across the world. The equipment is so scarce in some parts of the U.S. that the Centers for Disease Control and Prevention recently recommended that health care providers use “homemade masks” such as bandanas and scarves as a last resort to care for COVID-19 patients.
“Everybody in the country and most of the world is clamoring for the same scarce resources,” said Brian Labus, an assistant professor of epidemiology at UNLV. “We’re trying to get supplies that aren’t readily available.”
Nevada’s hospitals have a long-standing mutual aid agreement allowing them to transfer equipment, pharmaceuticals and even staffers to one another. Lake said the agreement has already been used during the COVID-19 outbreak to transfer protective equipment, mostly close-fitting N95 respirator masks.
Southern Nevada Health District officials declined to be interviewed for this story but wrote in a statement that they are coordinating requests for protective equipment with state and federal agencies.
If hospitals’ supplies of protective equipment are not replenished, doctors and other health care workers run a higher risk of contracting COVID-19. An outbreak among medical personnel could undermine Nevada’s hospitals from the inside.
“You can create all the capacity in your hospitals that you can, but it’s no good without a health care provider team,” UMC’s Asad said.
And for the sickest patients, there are concerns nationwide about meeting demand for ventilators, which are bedside machines that push oxygen into patients’ lungs.
At HCA Healthcare’s Nevada and California hospitals, intensive care has been necessary for about half of all in-patients with COVID-19, and “many of those patients are requiring time on a ventilator,” Corcoran said Tuesday.
There are about 880 ventilators at the state’s short-term acute care and critical access hospitals, close to a third of which were in use as of Friday, the NHA reported. Sisolak said the stock was far lower than it needs to be.
“We don’t have enough in any of our hospitals,” he said. “We’re doing the best we can in trying to acquire them on our own.”
McBride, the Valley Health System’s regional chief medical officer, said some of his hospitals’ other respiratory assistance machines could be converted into additional ventilators in an emergency, but that solution is also limited.
“This is not a supply that you can quickly manufacture and create a surplus of,” he said of ventilators. “There is a fixed number across our state’s hospital systems.”
No visitors in hospitals
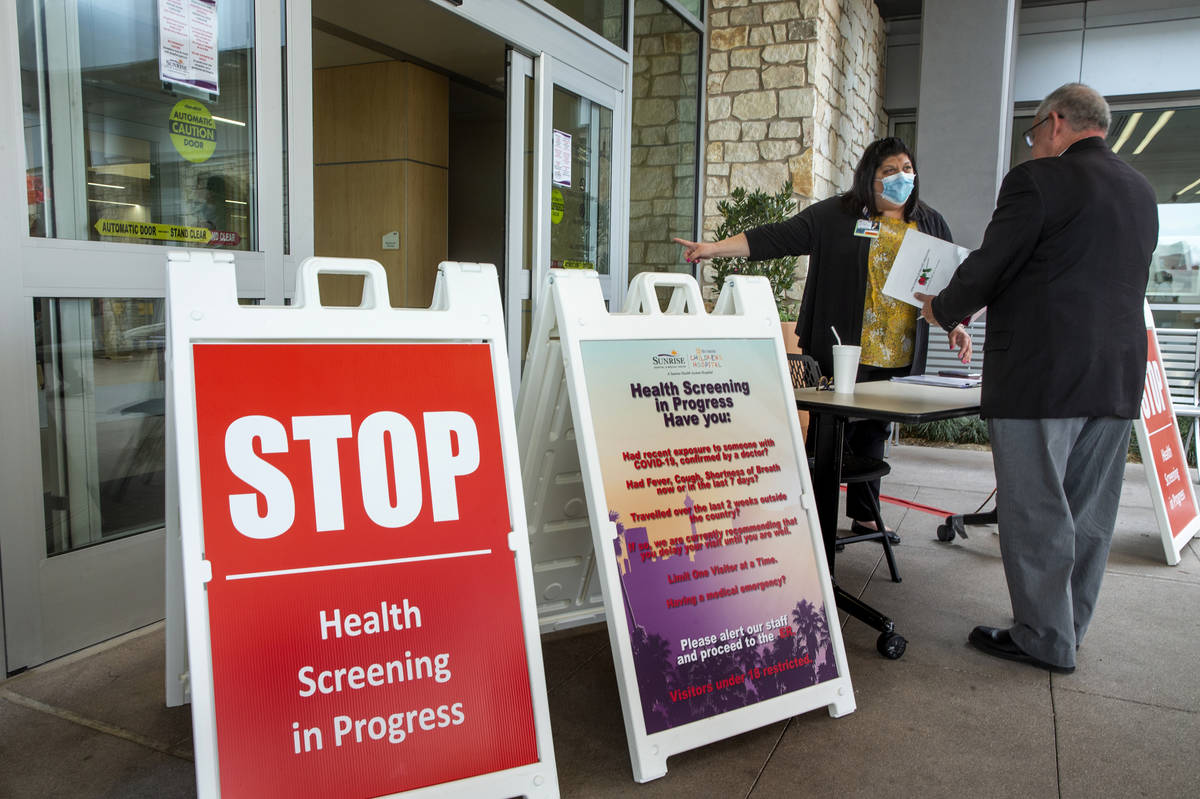
Local hospitals have already taken extraordinary steps to keep the disease from spreading to or from their facilities as they wait for a surge of COVID-19 patients.
On Wednesday and Thursday, the Las Vegas Valley’s largest hospitals enacted “no visitor” policies, allowing only a few exceptions.
HCA Healthcare’s Sunrise Hospital has erected white tents in its parking lot that can be used for evaluating people before they enter the hospital if they show symptoms of respiratory illness. This week, the company began measuring the temperature of everyone entering its local hospitals.
“We want to make sure we know who is inside our house, and we want to make sure they’re healthy,” Corcoran said.
HCA Healthcare is already treating in-patients confirmed or believed to have COVID-19 at all its Las Vegas Hospitals, Corcoran said. Patients exhibiting symptoms are placed in isolation rooms with antechambers for staffers to don protective equipment upon entry and discard it when they exit.
At Dignity Health-St. Rose Dominican hospitals, patients with symptoms are required to wear masks. UMC has designated an area of its hospital only for coronavirus patients, served by a dedicated staff of nurses and doctors.
The effectiveness of the efforts of health care providers and the public to slow the spread remains to be seen. Hospital operators are updating their preparedness plans in real time.
“Honestly, this is changing day to day, and sometimes hour to hour,” Corcoran said.
Update: This article was updated Saturday with newly released numbers from the Nevada Hospital Association.
Contact Michael Scott Davidson at sdavidson@reviewjournal.com or 702-477-3861. Davidson is a member of the Review-Journal’s investigative team, focusing on reporting that holds leaders and agencies accountable and exposes wrongdoing. Follow @davidsonlvrj on Twitter.
Clarification: A graphic in this story has been updated to include the number of Nevada adults projected to contract COVID-19 but not require hospitalization