Hospitals expected a dire situation. April data shows it never came.
Even at the height of Nevada’s novel coronavirus outbreak in early April, most local acute care hospitals never came close to being overwhelmed.
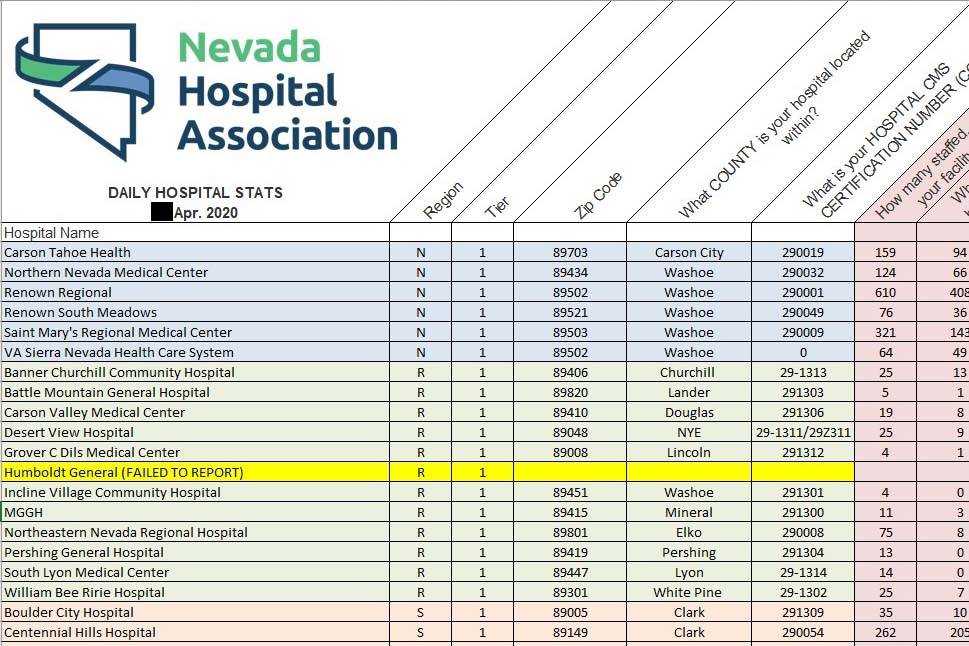
That’s according to newly released data from the Nevada Hospital Association, which for the first time offers a hospital-by-hospital breakdown of essential equipment usage, bed occupancy and staffing levels.
At Clark County’s acute care hospitals, the number of confirmed and suspected COVID-19 patients receiving treatment peaked at 633 people on April 7, the NHA data shows. On that day, more than 200 of those patients were receiving intensive care, and 160 were using mechanical ventilators to help them breathe.
“We absolutely saw a surge of coronavirus patients,” said Dr. Joe Corcoran, the chief medical officer overseeing Sunrise Hospital and Medical Center and other HCA Healthcare facilities in Nevada and California. “The good news is, we never felt the stress that we all feared when we were planning and making these preparations for the possibility of a dire situation.”
Overall, more than 1,300 people who have tested positive for COVID-19 in Clark County have received hospital treatment. Of those, 244 had died as of Tuesday afternoon.
In mid-March, state health officials feared a surge of coronavirus patients would inundate Nevada hospitals, pushing them past their capacity. Gov. Steve Sisolak and public health officials used the NHA data, compiled by the nonprofit in daily reports, to help them make critical decisions during the state’s outbreak.
But despite the initial fears, Nevada Chief Medical Officer Dr. Ihsan Azzam told the Review-Journal that social distancing measures stymied the virus’s spread and therefore lessened its impact on local hospitals.
“Initially, early modeling of case counts, severity and the need for surge capacity was troubling, but due to a quick response and the work of all Nevadans to help flatten the curve, our hospitals have not been overwhelmed with patients,” he wrote in a statement.
Most acute care hospitals never approached reaching their capacity, nor did they have serious issues keeping their facilities staffed. And while there was overwhelming global demand for face masks and other protective gear, only one major hospital in Clark County reported having a severe shortage across its inventory.
The county has about 4,500 staffed hospital beds spread across its short-term acute care and critical access hospitals, according to the NHA report. Those facilities have about 600 ICU rooms and about 700 ventilators.
The newspaper obtained the reports through a public records request. The NHA, which reportedly sought to shield the reports from public view, declined to answer a Review-Journal reporter’s questions about the documents in an interview or by email.
“We are pleased that the data provided by the Nevada Hospital Association on behalf of our member hospitals has helped the Governor and our state’s healthcare partners guide decisions in the fight against the COVID-19 pandemic and aid in reopening Nevada,” NHA spokeswoman Amy Shogren wrote in an emailed statement. “We look forward to continuing to provide this valuable information to further assist with key decisions.”
But while the reports contain mostly good news, they also show certain hospitals faced challenges.
Some reported their intensive care rooms were nearly full for the entire month. Others reported staff quit or took leave because they feared contracting the coronavirus. A small number had to convert anesthesia or BiPAP machines into ventilators, although it’s unclear if they were ever used.
Two hospitals also confirmed to the Review-Journal that they mistakenly misreported the number of doctors and ICU nurses they had out sick, in one case inflating the number more than tenfold for almost the entire month of April.
One southwest Las Vegas Valley hospital faced particular difficulties with keeping protective gear in stock, the NHA reports show.
The reports categorize hospitals’ staffing levels and protective gear inventories in a “stoplight” system. Green represented an appropriate amount; yellow indicated the risk of a shortage; and red signaled critically low levels.
The San Martin campus of Dignity Health’s St. Rose Dominican Hospital operated with “red” levels of protective gear during the first half of April, reporting that it had severe shortages of masks, gowns, gloves and testing kits. Supplies at the facility reached “near critical” levels after it was unable to secure enough protective gear from private and government suppliers, Dignity Health spokesman Gordon Absher wrote in an email.
The hospital system’s Siena campus, located in Henderson, reported that its ICU beds were near and at capacity for almost all of April. The facility began hiring nurses for short-term assignments in its ICU and emergency department in early April after staffing levels in those departments reached “red” levels for a single day on April 6.
The Siena campus also vastly over-reported the number of doctors and ICU nurses it had out sick, Absher wrote in an email.
Throughout the month it reported having between 41 to 83 employees out sick. However, the actual number never rose above four. Among the sick were a doctor and nurse from the hospital, who became critically ill after treating infected patients.
“We continue to look into the circumstances, but this initially appears to be a simple misreading of the request, which was then repeated each subsequent day,” Absher wrote.
Dignity Health officials declined to be interviewed about the reports, but Nevada market president Lawrence Barnard wrote in a statement that there was no reason for alarm.
“These daily reports may be viewed by some as a reflection of how close to the edge we came,” Barnard wrote. “We choose to view them, not as cause for concern, but as testament to the efforts and resourcefulness demonstrated by the health care industry and the extraordinary professional achievement of our people to serve this community and keep our neighbors safe.”
Reporting guidelines caused confusion
Officials at other hospitals said the reports’ data could be misinterpreted.
Valley Health System’s Henderson Hospital reported that it operated near and above capacity for much of the second half of April. On April 19, the hospital reported its total number of inpatients, including those not infected with coronavirus, exceeded its staffed, acute care beds by 10 people.
Henderson Hospital also reported that its ICU rooms were 90 percent or more full for almost all of April. So did Spring Valley Hospital, another Valley Health System facility.
But the two hospitals were actually never at risk of overcrowding, Valley Health System regional vice president Karla Perez said. The hospitals had more beds, and even more surge capacity, but they were staffed based on their current number of inpatients.
“The question (on the NHA report) probably could have been worded a bit better,” Perez said. “At no point did they ever hit 100 percent (capacity) in the month of April. I think the highest they hit was 85 percent.”
Hospital staffers quit
Some of the county’s hospitals reported losing staff because of the pandemic.
Spring Valley Hospital reported on multiple days in mid-April that its ICU nurses and other staff members were resigning to take advantage of “financial incentives” offered by hospitals in New York and California. Others were leaving the hospital because of “COVID fears,” according to the NHA’s April 15 report.
Perez said fewer than 10 staff members opted to take temporary, high-paying assignments in parts of the U.S. that were among the hardest hit by the coronavirus, but they were expected to return to Las Vegas when the Valley Health System asked them to. Others chose to be voluntarily furloughed because they or their family members were at greater risk of serious complications from infection.
“There was nothing alarming or concerning about the turnover,” she said.
A North Las Vegas hospital faced its own bout of staff resignations in early April.
North Vista Hospital stated that registered nurses, certified nursing assistants and technicians left over “concern of COVID exposure,” according to the NHA reports. Other staff members submitted requests to take unpaid leave for family and medical reasons.
Hospital officials declined an interview but provided a written statement through spokeswoman Susan Olson.
“These are uncertain and stressful times for everyone,” Olson wrote. “People have to make decisions that are best for themselves and their families, and we must support those decisions while also ensuring that our hospital has the staff and resources to care for this community. And we do.”
Contact Michael Scott Davidson at sdavidson@reviewjournal.com or 702-477-3861. Davidson is a member of the Review-Journal’s investigative team, focusing on reporting that holds leaders and agencies accountable and exposes wrongdoing. Follow @davidsonlvrj on Twitter.