California gets ready for possible winter pandemic surge
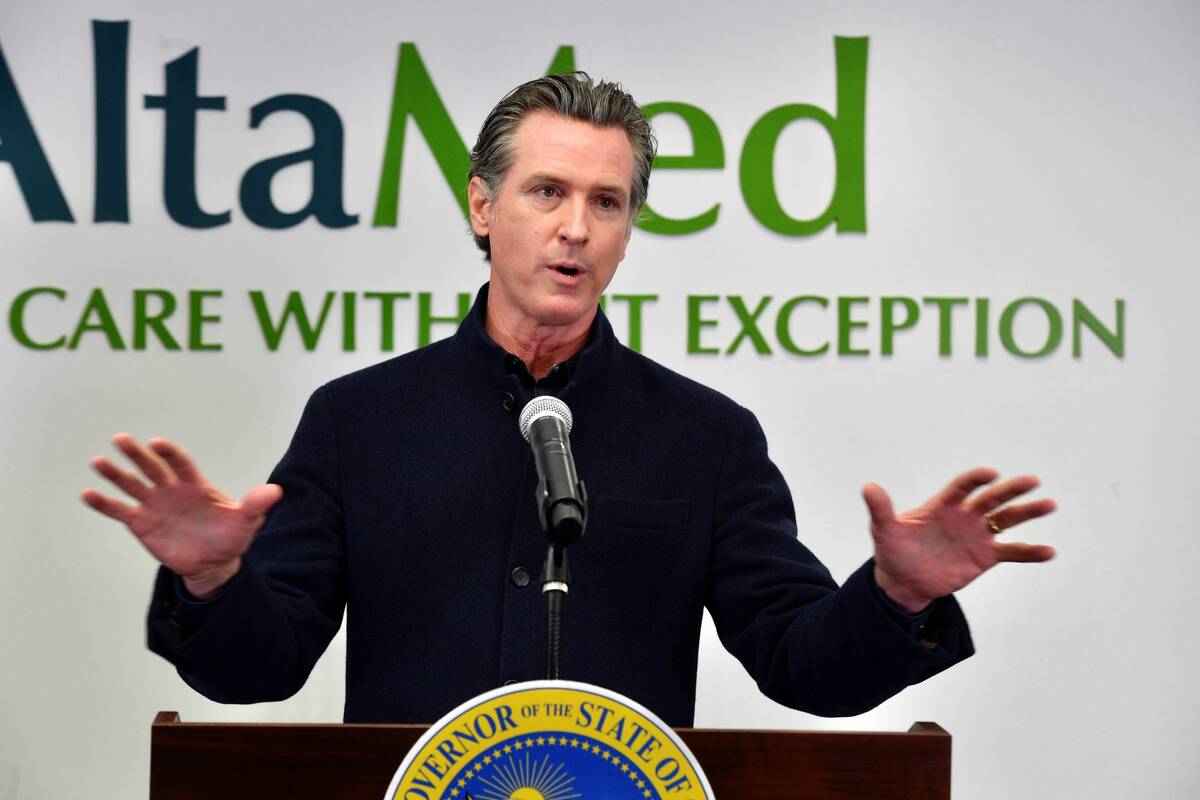
LOS ANGELES — California has begun positioning equipment and locking in contracts with temporary health care workers in preparation for another possible winter surge of coronavirus cases, Gov. Gavin Newsom said Wednesday.
The most populous state in the country still is doing comparatively well with the rest of the U.S. in terms of cases and hospitalizations. But Newsom warned Californians should prepare for another harsh pandemic winter even though the state is among the nation’s leaders with about 74% of eligible people with at least one dose of the vaccine.
While statewide hospitalizations have fallen by about half since a summer peak at the end of August, they have started creeping up in some areas, particularly the Central Valley and portions of Southern California including Los Angeles and San Bernardino counties.
“We’ve seen some signs that suggest concerns,” Newsom said.
California earlier this fall had the nation’s lowest case rate but is now 16th, he said, while the positivity rate for those tested is 2.3% after falling below 1% in June.
Newsom signed an executive order that through March 31 will continue to allow out-of-state medical workers to treat patients in California and allow emergency medical technicians and others to keep administering vaccines and providing other related services. It also keeps flexibility for health care facilities, for instance allowing parking lots to be used for vaccination sites.
Beyond the upward trend in certain parts of the state, state health officials said they are generally apprehensive because colder weather will keep people inside. There will be more holiday mingling at a time when vaccine and natural immunity acquired months ago will begin to wane unless more people get booster shots.
“We have learned over the last two years that COVID-19 takes advantage when we put our guard down,” Newsom’s health department said in a statement.
Concerns grow
The state’s own models still predict an overall decline in hospitalizations and intensive care cases over the next month. And the statewide R-effective that measures infection rates also continues dropping and now is at 0.85. Anything below 1 means the number of infected persons will decrease.
The concern is that even those who are vaccinated may be more vulnerable to the extremely contagious delta variant unless many more people get booster shots, which currently are lagging, said Dr. Kirsten Bibbins-Domingo, a professor of epidemiology at the University of California, San Francisco.
Moreover, California is so large and geographically and demographically diverse that conditions are “wildly variable,” which also affects the state’s modeling at a time when many have grown tired of precautions like masking and isolating, she said.
“There are plenty of local models that do show rising hospitalizations that we are already starting to see in local environments,” Bibbins-Domingo said. “It is a little bit of a race, and it sort of depends on whether waning immunity wins or whether us getting boosters into people wins.”
Newsom used a visit to a COVID-19 vaccine and flu shot clinic in Los Angeles to urge residents, including newly eligible children 5 to 11, to get vaccinated. He also urged booster shots for those who are eligible.
Newsom, who got a booster on Oct. 27, said it has become evident from the experience of Europe and other U.S. states that the coronavirus has a seasonal aspect that can lead to an increase in infections.
He used apocalyptical reminders of last year’s winter surge that had officials buying body bags and bringing mobile morgues to Southern California as infections surged 10-fold over eight weeks and overwhelmed many hospitals.
“Thousands of people lost their lives, thousands of people on life support, close to death,” he said. That’s why state officials are “doing everything in our power to prepare.”
Staffing challenges
Brian Ferguson, a spokesman for the Governor’s Office of Emergency Services, said the state’s preparations since the start of the pandemic have “put the state in a much better place to withstand any surge that occurs this winter.”
The state “has all of the expanded capacity from the mobile field hospitals and supply caches that were acquired during the pandemic as well as the contracts to bring in nursing and medical personnel that were put in place previously,” Ferguson said.
Stephanie Roberson, government relations director of the California Nurses Association, said the Health and Human Services Agency “has been working super closely with the hospitals to make sure that they are getting staff.”
That includes extending an out-of-state staffing waiver and in-state waivers for nurses to work as teams. Roberson expects the state to soon start spending money help with hiring temporary employees, as it did before as hospitals were stretched to the breaking point last winter.
The California Hospital Association is in regular communication and working collaboratively with state health officials as cases rise in parts of the state, said spokeswoman Jan Emerson-Shea.
Hospital staffing shortages are already a concern in some areas, Bibbins-Domingo said.
“The challenge is that the areas that are least vaccinated are also the areas that are least able to withstand a surge, which are oftentimes our rural areas” and denser, poorer urban areas, she said. “It is prudent to plan for that for some extent, just because where we are more likely to see it is going to be in those areas that are least able to withstand it.”