Some of Nevada’s ‘superbug’ cases found at 2 Las Vegas hospitals
Cases of once-rare “superbug” Candida auris have climbed to 600 in Southern Nevada, with more than one-third identified at just two hospitals.
Sunrise Hospital and Medical Center, the largest general acute-care hospital in the state, has reported 122 cases of the drug-resistant fungus, the most of any hospital or skilled nursing facility. The first pediatric cluster of C. auris cases in the U.S. was identified at the Las Vegas hospital in May.
Horizon Specialty Hospital — Las Vegas reported 95, the second-highest number, according to state data as of Oct. 24. Thirty-three medical facilities have now reported cases.
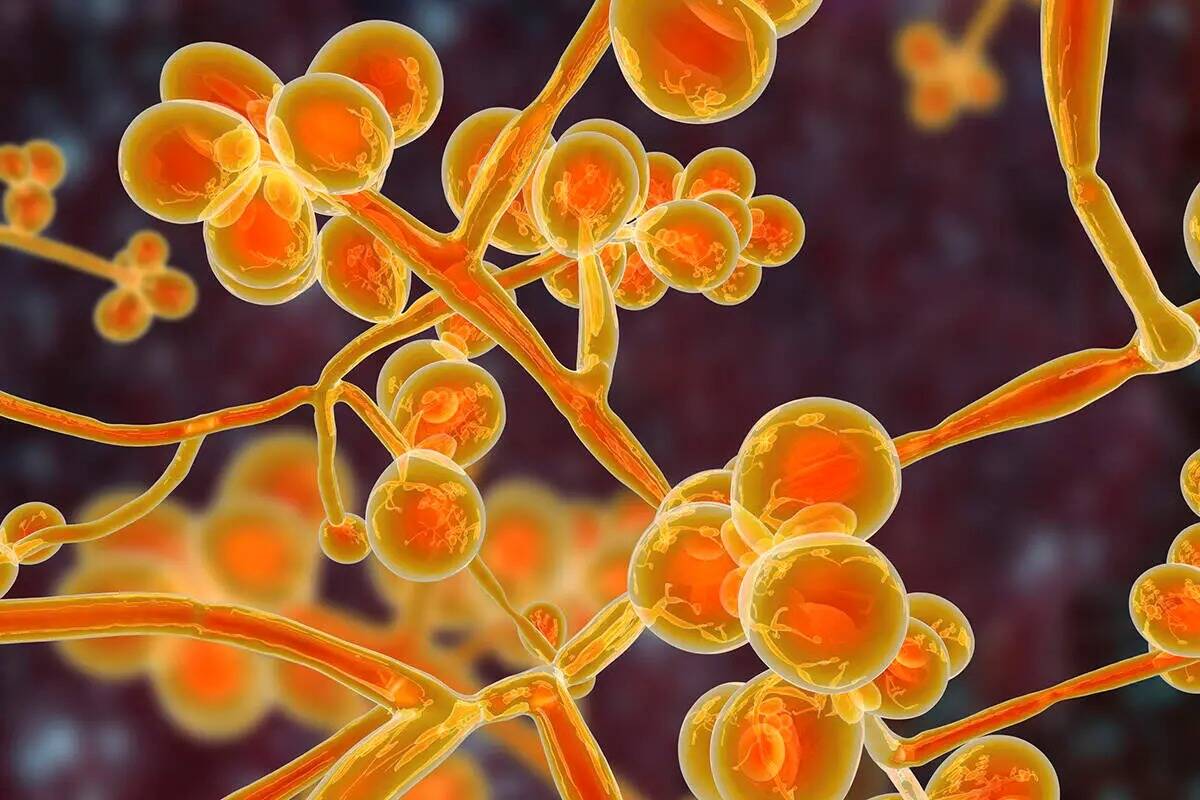
C. auris can cause bloodstream infections and even death, particularly in hospital and nursing home patients with serious medical problems. More than one in three patients die after developing an invasive infection, such as one affecting the blood, heart or brain, according to the Centers for Disease Control and Prevention.
As of Nov. 18, 63 deaths had been reported in patients with C. auris, state health officials said. The first cases ever identified in Nevada were reported in August of last year.
Rounding out the five facilities reporting the most cases are Horizon Specialty Hospital of Henderson with 59 cases, Valley Hospital Medical Center with 38, and Silver Ridge Health Center with 32, according to Nevada Department of Health and Human Services data.
A higher number of cases at a facility “doesn’t always mean there’s a problem with infection control,” said Kimisha Causey with the Nevada State Healthcare Associated Infection Program. The facility reporting a case may not be the place where the patient acquired it, she said, noting that patients transfer among facilities.
She acknowledged about higher case numbers, however, “From a consumer standpoint, to me it would be concerning.”
Hospitals said some of the cases they are reporting are those they identify through screening patients upon admission.
“With a focus on heightened surveillance testing, we continue to identify patients upon admission,” said Dr. Steven Merta, chief medical officer for Sunrise Hospital. “We continue to practice targeted testing, enhanced isolation, high-level cleaning practices and advanced infection prevention technologies to keep our patients, colleagues and visitors safe.”
Gretchen Papez, a representative of Valley Health System hospitals including Valley Hospital, said their hospitals “remain vigilant in the detection and treatment of C. auris through screening, testing, treatment, isolation protocols and room disinfection processes with deep cleaning and UV-C lights.”
Horizon Specialty Hospitals and other facilities reporting relatively high case numbers did not respond to requests for comment.
Long-term patients most vulnerable
Genetic analysis of cases indicates that there are two separate outbreaks of C. auris in Southern Nevada, each with a different clade, or strain, of the fungus, said Mark Pandori, director of the Nevada State Public Health Laboratory in Reno.
It appears that two facilities were struck by different strains of the fungus, which then spread to other facilities, Pandori said.
These facilities were Sunrise and Centennial Hills Hospital Medical Center, Shannon Litz, a health department public information officer, said last week.
With cases mounting, the state health department in April launched an investigation. The CDC sent a team to assist with the outbreaks, including with assessing facility infection control practices and educating staff on the new pathogen and how to prevent its spread.
The basics: C. auris is highly transmissible. It spreads through contact with contaminated surfaces. It also spreads from person to person. It spreads from facility to facility through patients and potentially staff.
It is hard to identify. Some people become colonized with the fungus, which dwells in the folds of their skin, invisible to the eye and causing no symptoms. Colonized people can spread the germ even though they don’t feel sick.
It is hard to treat. Anti-fungal medications don’t always work.
The proper use of personal protection equipment, including gloves and gowns, and of other infection-control procedures, from basic hand-washing to high-tech cleaning protocols, can curb its spread.
People most likely to become infected with C. auris are those who have been hospitalized in a health care facility for a long time, have a central venous catheter or other lines or tubes entering their body, the CDC said.
Roni Johnson said her 65-year-old brother, Randy Hull, tested positive for C. auris after having a stroke a year ago and transferring among a handful of different hospitals and long-term care facilities.
The stroke cost the retired trucker his ability to walk, talk and swallow, and also led to pneumonia. In March, he transferred to Kindred Hospital Las Vegas – Sahara, where he was weaned off a ventilator. He was talking, watching ball games and able to sit in a chair with assistance, Johnson said. Then in October, he got sicker and sicker.
“All of a sudden he took a turn, and there weren’t any answers,” she said. “If I had not gotten him out of there, hands down he would have died.”
Johnson had her brother transferred to MountainView Hospital, where he was diagnosed with a C. auris blood infection, a urinary tract infection and pneumonia, she said. He since has improved and been transferred to a long-term care facility in Utah.
Because of privacy issues, Kindred Hospitals said it could not comment on the condition or treatment of a current or former patient.
Kindred Hospitals have strict infection control protocols and best-practice training “to ensure our practices are best in class, especially to protect our most vulnerable patients from drug resistant organisms,” the organization said in a statement.
It also said Kindred Hospitals test all patients for C. auris upon admission, isolating them until test results are known.
Eleven colonization cases and four clinical cases have been reported at the Kindred Sahara hospital, said Dawn Cribb, a state health department public information officer.
Testing not required
Based on CDC guidance, the Nevada health department recommends that facilities screen new patients for C. auris upon admission. It also recommends that patients again be tested if their roommate or another patient in their unit tests positive, Causey said.
However, not all facilities are consistently following the recommendations, Causey said, though she said she could not immediately name those that were not. Under Nevada law, the health department cannot mandate screenings and testing, she said.
Numbers of new reported cases have been declining since September, according to health department data. However, this may reflect a decline in screening.
“Countywide, the cases appear to be declining,” Cribb said. “However, please note that the volume of screening is not as much as in earlier months.”
Contact Mary Hynes at mhynes@reviewjournal.com or 702-383-0336. Follow @MaryHynes1 on Twitter.