Secrecy, fear rampant in local nursing homes where COVID-19 is too
“I could have it, for all I know.”
That was just one of the comments the Review-Journal heard this week from residents of Las Vegas Valley nursing and assisted living homes, which are being hard hit by COVID-19.
The number of deaths in the state-regulated homes has risen more than 155 percent since the state reported 18 fatalities through a new tracking tool unveiled in mid-April.
As of Friday, COVID-19 had killed 51 residents and two staff members in the homes, accounting for nearly 21 percent of the state’s death toll from the disease. Cases have been reported in 61 of the 461 homes in the state.
Despite such alarming numbers and the fact that the elderly, many of whom have pre-existing health conditions, are among the most vulnerable to the new coronavirus, the operators of those homes have been publicly silent about what measures they are taking to stop the spread of the disease.
Attempts by the Review-Journal to interview officials at some of those homes were rebuffed, and calls seeking comment from others were not returned.
Residents, family members and staffers at some of the hardest-hit homes in the Las Vegas Valley said that they, too, are unable to get answers to even the most basic questions about what’s going on.
In an effort to pierce the shroud of secrecy, here are a few of the stories they shared about life inside these battlegrounds of the pandemic.
‘Abdicating their responsibility’
It is no secret that Barbara Tinch contracted COVID-19 at the Heights of Summerlin.
The 86-year-old had been confined to her room at the Las Vegas nursing home for more than a month under a quarantine intended to keep the disease at bay when she suddenly came down with a fever that spiked at 105 degrees. Soon she felt a pang in her chest and began struggling to breathe.
“I’m in so much pain I’m going to die,” she told her daughter, Lisa, by phone.
Lisa Tinch said that conversation occurred April 10, when her mother called from an isolation ward for coronavirus patients. It was the first time her family knew that the virus had infiltrated the facility.
Three days later, Barbara Tinch was in the intensive care unit at Southern Hills Hospital, where she was tested for COVID-19.
Her daughter said the home’s nursing director called her for the first time the following day, not to share words of comfort but to convey a warning: If her mother tested positive, she would not be permitted to return to the Heights when she was discharged.
Later that week, Barbara Tinch tested positive.
As soon as she learned that her mother was in an isolation ward at the home, Lisa Tinch spent the weekend trying to reach nursing staffers about her mother’s condition. She finally succeeded April 12.
“She said, ‘I can’t take care of phone calls if I’m all garbed up in (personal protective equipment) taking care of the patients. I can either do one or the other, but I can’t do both,’ ” said Tinch, who is a nurse herself.
To this day, Tinch said, the Heights has never told her how many COVID-19 cases have been reported at the home. If she had looked at the state data on Friday, she would have been appalled. The home now has 98 cases, the most in the state, and five residents have died.
When the state’s reporting tool debuted April 13, the Heights had only four cases and one death.
Repeated requests for comment from the Heights of Summerlin and its corporate owner, Summit Care LLC, were not returned.
The lack of communication from officials and staffers at the home is what infuriates Lisa Tinch.
“I just wanted to get an update, even if it was once a day,” she said. “They’re abdicating their responsibility as an advocate for elderly.”
‘No masks for six weeks’
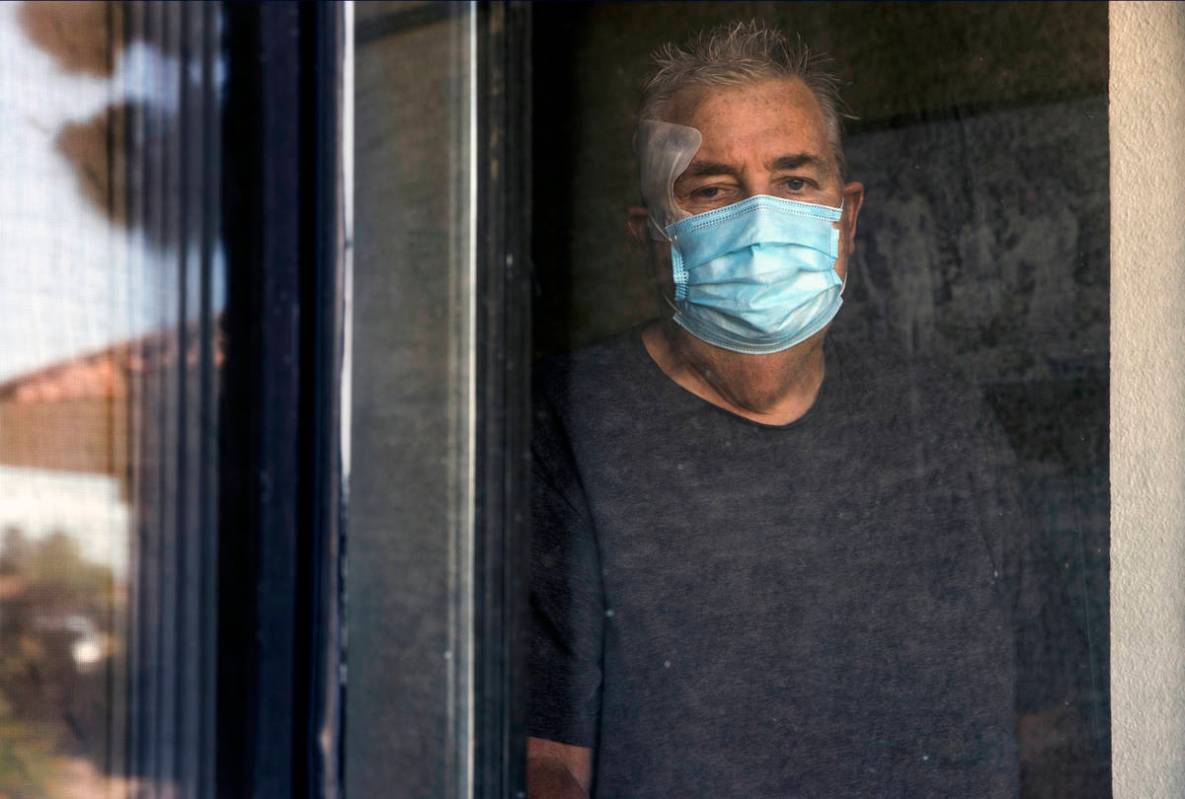
Richard Haacke, 61, said he remains fearful about living at the College Park Rehabilitation Center in North Las Vegas, despite having received a negative result Tuesday from a COVID-19 test he took last week.
“I’ve been exposed to five people. I know that,” Haacke said, referring to fellow patients at the facility who he knows have been diagnosed with the disease. He then noticed his normal caregivers had stopped coming to work.
“I asked them, ‘You don’t think it would be helpful for me to know that the woman who has been in my room, put a mask on my face and gives me a breathing treatment has it?’” he said, adding that his inquiries were dismissed.
Haacke requires breathing treatments around the clock and suffers from kidney failure, heart disease and anxiety. On Wednesday, he said his roommate was given a nasal test for the coronavirus.
State data shows that as of Friday, the facility had seven confirmed cases of COVID-19 among staff members and four among residents.
A letter sent to family members and residents a week after the first cases at the facility were reported didn’t specify how many, nor did it alert residents who might have been exposed.
“They’re not giving all the details. That’s my biggest gripe, and they waited so long to tell us,” Haacke said. “They had no masks for six weeks, and then all of a sudden they look like they’re in a hazmat costume,” he said.
Repeated phone calls to College Park and its corporate owner, Thi of Nevada at Cheyenne LLC, for this story were not returned.
But Haacke said staffers didn’t start having their temperatures checked before entering until April 1. Now they are calling in sick, and staffers have started blocking off hallways with plastic sheets for makeshift isolation units, he said. Only on Thursday, he said, did the facility start mass testing staff members and residents.
“I could have it, for all I know,” he recalls one staff member telling him days ago while he was cleaning the area.
“Don’t let anybody touch you,” another whispered in his ear.
‘It would scare the patients’
Despite the lack of personal protective equipment, many homes in the state aren’t providing proper education to staffers and refuse to inform them of infected residents, a certified nursing assistant told the Review-Journal in an email.
“I’ve never had a face shield or an N95 mask while working in any of these facilities,” wrote the woman. “At one point I was informed by fellow medical professionals that they were not allowed to wear a mask while at work for fear it would scare the patients.”
The Review-Journal is not naming the nursing assistant because she said she fears retribution from her employer for speaking out.
“The people I work alongside of are forgotten. You take what you are given and you do the best you can, and if all else fails we have each other to cry with,” she said. “They may not be one the front lines in the ER, but they are on the front lines to protect our most vulnerable citizens.”
Most of the homes in the state are represented by the Nevada Health Care Association.
Brett Salmon, who is president of the association as well as president of one of its members, the Nevada Center for Assisted Living, said in a statement that a lack of test kits and personal protection equipment has contributed to the current situation.
He said he couldn’t comment on specific incidents, but he noted that “long-term care facilities are required to provide family notification, resident notification and notification to the resident’s authorized responsible party.”
The Centers for Medicare and Medicaid Services is also coming out with some guidance related to notifications, and the cases in Nevada have been reported to the counties and the state, he said.
“Our caregivers are deeply concerned for the health and well-being of the residents they care for,” he said. “Every day, long-term health care workers are taking risks by going to work.”
Salmon emphasized that broad-based testing is vital to mitigating the spread in these homes, and the association has been told that there’s a “plan to do such testing in the next several weeks.”
Ombudsman locked out
One resource available to nursing and assisted living home residents and their families is the state’s Long Term Care Ombudsman Program, which reviews complaints and advocates for senior residents of long-term care facilities and their families.
Placing a family member in such facilities and trying to ensure they receive quality care is a worry in the best of times, ombudsman Jennifer Williams-Woods said. But a lack of communication during something like the coronavirus pandemic can “exacerbate that fear.”
But Williams-Woods said the agency’s caseload has dwindled because the team has been unable to visit residents at facilities in person since early March.
One recent case in which the program did intervene was that of Barbara Tinch. When the office approached the Heights of Summerlin in response to her daughter’s complaint about the threat to prevent her from returning after her discharge from the hospital, the facility agreed to readmit her after she completes a stay in a long-term acute care hospital.
“That has been a concern, and we are trying to reach out to facilities to make sure they are taking folks back. That is a requirement regardless of what they are in the hospital for,” Williams-Woods said. “We will continue to advocate for those individuals and continue to educate.”
Contact Briana Erickson at berickson@reviewjournal.com or 702-387-5244. Follow @ByBrianaE on Twitter.