6 tips to stay safe from COVID this winter
Last year, the emergence of the highly transmissible omicron variant of the COVID-19 virus caught many people by surprise and led to a surge in cases that overwhelmed hospitals and drove up fatalities. Now we’re learning that omicron is mutating to better evade the immune system.
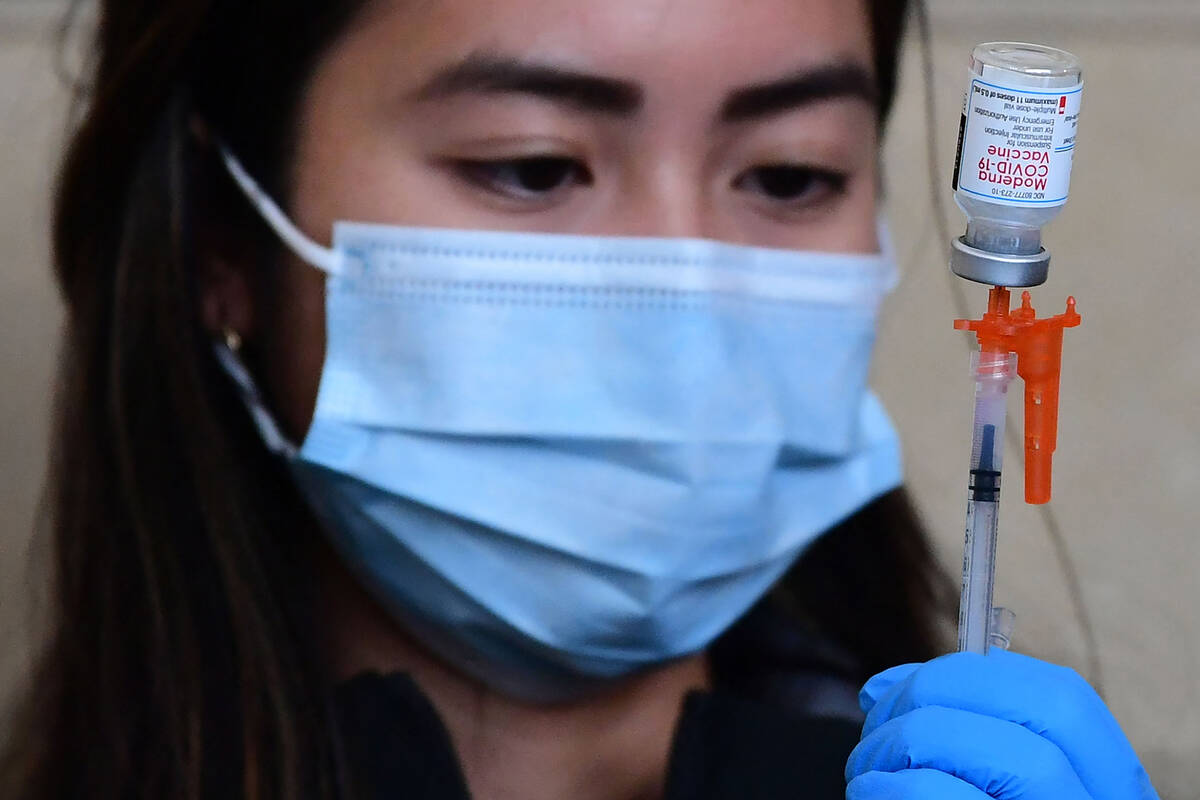
Omicron-specific vaccines were authorized by the FDA in August and are recommended by U.S. health officials for anyone 5 or older. Yet only half of adults in the United States have heard much about these booster shots, according to a recent Kaiser Family Foundation poll, and only a third say they’ve gotten one or plan to get one as soon as possible. In 2020 and 2021, COVID cases spiked in the U.S. between November and February.
Although we don’t know for sure that we’ll see another surge this winter, here’s what you should know about COVID and the updated boosters to prepare.
1. Do I need a COVID booster shot this fall?
If you’ve completed a primary vaccination series and are 50 or older, or if your immune system is compromised, get a COVID booster shot as soon as possible. Forty percent of deaths are occurring among people 85 and older and almost 90 percent among people 65 and over. Although people of all ages are being hospitalized from COVID, those hospitalizations are also skewing older.
Unvaccinated people, while in the minority in the U.S., are still at the highest risk of dying from COVID. It’s not too late to get vaccinated ahead of this winter season.
If you’ve already received three or more COVID shots, you’re 12 to 49 years old and you’re not immunocompromised, your risk of hospitalization and death from the disease is significantly reduced and additional boosters are not likely to add much protection.
However, getting a booster shot provides a “honeymoon” period for a couple of months after vaccination, during which you’re less likely to get infected and thus less likely to transmit the virus to others. If you’ll be seeing older, immunocompromised or otherwise vulnerable family and friends over the winter holidays, you might want to get a booster two to four weeks in advance to better shield them against COVID.
You may have other reasons for wanting to avoid infection, such as not wanting to have to stay home from work because you or your child is sick with COVID. Even if you aren’t hospitalized from COVID, it can be costly to lose wages or arrange for backup child care.
One major caveat to these recommendations: You should wait four to six months after your last COVID infection or vaccination before getting another shot. A dose administered too soon will be less effective because antibodies from the previous infection or vaccination will still be circulating in your blood and will prevent your immune cells from seeing and responding to vaccination.
2. Do kids need to be vaccinated even if they’ve had COVID?
Although children are at lower risk for severe COVID than adults, the stakes for kids are higher than many diseases already recognized as dangerous. Their risk shouldn’t be measured against the risk that COVID poses to other age groups but against the risk they face from other preventable diseases. In the first two years of the pandemic, COVID was the fourth- or fifth-leading cause of death in every five-year age bracket from birth to 19, killing almost 1,500 children and teenagers. Other vaccine-preventable diseases such as chickenpox, rubella and rotavirus killed an average of about 20 to 50 children and teens a year before vaccines became available. By that measure, vaccinating kids against COVID is a slam dunk.
Children who have had COVID also benefit from vaccination. The vaccine reduces their risk of hospitalization and missing days of school, when parents might need to stay home with them.
But it’s precisely because the stakes are higher for kids that many parents are anxious about getting their children vaccinated. As recently as July, just after the FDA authorized COVID vaccines for children as young as 6 months, a KFF poll found that over half of parents of children under age 5 said they thought vaccines posed a greater risk to the health of their child than getting the disease. And in the most recent poll, half said they had no plans to get their children vaccinated. COVID vaccination rates range from 61 percent among children ages 12 to 17 to 2 percent among kids younger than 2.
Similar to influenza, COVID is most deadly for the very youngest and oldest. At especially high risk are infants. They’re unlikely to have immunity from infection, and a small share have been vaccinated. Unless their mothers were vaccinated during pregnancy or got COVID during pregnancy — the latter of which poses a high risk of death for the mother and of preterm birth for the baby — infants are probably not getting protective antibodies against COVID through breast milk. And because infants have small airways and weaker coughs, they’re more likely to have trouble breathing with any respiratory infection, even one less deadly than COVID.
3. Will I need a COVID shot every year?
It depends on the targets set by public health officials whether COVID becomes a seasonal virus like the flu and how much the virus continues to mutate and evade humanity’s immune defenses.
If the goal of vaccination is to prevent severe disease, hospitalization and death, then many people will be well protected after their primary vaccination series and may not need additional shots. Public health officials might strongly recommend boosters for older and immunocompromised people while leaving the choice of whether to get boosted to those with lower risk. If the goal of vaccination is to prevent infection and transmission, then repeat boosters will be needed after completing the primary vaccination series and as often as a couple of times a year.
Influenza is a seasonal virus causing infections and disease generally in the winter, but scientists don’t know whether COVID will settle into a similar, predictable pattern. In the first three years of the pandemic, the United States has experienced waves of infection in summer. But if the COVID virus were to become a wintertime virus, public health officials might recommend yearly boosters. The Centers for Disease Control and Prevention recommends that people 6 months and older get a flu shot every year with very rare exceptions. However, as with the flu, public health officials might still place a special emphasis on vaccinating high-risk people against COVID.
And the more the virus mutates, the more often public health officials may recommend boosting to overcome a new variant’s immune evasion.
4. Are more COVID variants on the way?
The omicron variant has burst into an alphabet soup of subvariants. The BA.5 variant that surfaced this year remains the dominant variant in the U.S., but the BA.4.6 omicron subvariant may be poised to become dominant in the United States. The BA.4.6 omicron subvariant is better than BA.5 at dodging people’s immune defenses from both prior infection and vaccination.
In other parts of the world, BA.4.6 has been overtaken by BA.2.75 and BF.7 (a descendant of BA.5). The BA.2.75.2 omicron subvariant drove a wave of infections in South Asia in July and August. Although the U.S. hasn’t yet seen much in the way of another variant descended from BA.5 — BQ.1.1 — it is rising quickly in other countries like the U.K., Belgium, and Denmark. The BA.2.75.2 and BQ.1.1 variants may be the most immune-evasive omicron subvariants to date.
BA.4.6, BA.2.75.2, and BQ.1.1 all evade Evusheld, the monoclonal antibody used to prevent COVID in immunocompromised people who don’t respond as well to vaccination. Although another medication, bebtelovimab, remains active in treating COVID from BA.4.6 and BA.2.75.2, it’s ineffective against BQ.1.1. Many scientists are worried that Evusheld will become useless by November or December. This is concerning because the pipeline for new antiviral pills and monoclonal antibodies to treat COVID is running dry without a guaranteed purchaser to ensure a market. In the past, the federal government guaranteed it would buy vaccines in bulk, but funding for that program has not been extended by Congress.
Other omicron subvariants on the horizon include BJ.1, BA.2.3.20, BN.1, and XBB, all descendants of BA.2.
It’s hard to predict whether an omicron subvariant or yet another variant will come to dominate this winter and whether hospitalizations and deaths will again surge in the U.S. Vaccination rates and experience with prior infections vary around the world and even within the United States, which means that the different versions of omicron are duking it out on different playing fields.
While this might all sound grim, it’s important to remember that COVID booster shots can help overcome immune evasion by the predominant omicron subvariants.
5. What about long COVID?
Getting vaccinated does reduce the risk of getting long COVID, but it’s unclear by how much. Researchers don’t know if the only way to prevent long COVID is to prevent infection.
Although vaccines may curb the risk of infection, few vaccines prevent all or almost all infections. Additional measures — such as improving indoor air quality and donning masks — would be needed to reduce the risk of infection. It’s also not yet known whether prompt treatment with currently available monoclonal antibodies and antiviral drugs such as Paxlovid reduce the risk of developing long COVID.
6. Do I need a flu shot, too?
The CDC recommends that anyone 6 months of age or older get an annual flu shot. The ideal timing is late October or early November before the winter holidays and before influenza typically starts spreading in the U.S. Like COVID shots, flu shots provide only a couple of months of immunity against infection and transmission, but an early flu shot is better than no flu shot.
It’s especially important for people 65 or older, pregnant women, people with chronic medical conditions and children under 5 to get their yearly flu shots because they’re at highest risk of hospitalization and death. Although younger people might be at lower risk for severe flu, they can act as vectors for transmission of influenza to higher-risk people in the community.
High-dose flu vaccines and “adjuvanted” flu vaccines are recommended for people 65 and older. Adjuvants strengthen the immune response to a vaccine.
It is safe to get vaccinated for COVID and the flu at the same time, but you might experience more side effects such as fevers, headaches or body aches.